
Imagine this: you lie awake at 3 a.m., every night, because your back hurts. You finally drift off, but wake up three hours later with your muscles screaming. The next day, your pain feels worse-not just because of the injury, but because you didn’t sleep. So you try another pill. It helps a little, but leaves you groggy. The next night, the pain is even worse. And the cycle keeps going.
This isn’t just bad luck. It’s a well-documented biological loop called the insomnia-pain cycle. And it traps millions of people with chronic pain. You’re not broken. You’re caught in a system where pain ruins sleep, and sleep loss makes pain worse. It’s not one causing the other-it’s both feeding each other, like a fire that won’t go out.
How Pain Kills Sleep (And Why It’s Not Just Discomfort)
People think pain keeps you awake because it’s uncomfortable. That’s true-but it’s only half the story. Chronic pain doesn’t just interrupt sleep; it rewires how your brain processes rest.
When you have ongoing pain, your nervous system stays on high alert. Even when you’re lying still, your body is bracing for more discomfort. This keeps your stress hormones-like cortisol-elevated. Your brain never fully switches into deep sleep mode. You might spend hours in bed, but your sleep is shallow, fragmented, and full of micro-awakenings you don’t even remember.
Research shows people with chronic pain take 25-30 minutes longer to fall asleep. Once asleep, they wake up 40-50% more often than people without pain. On average, they lose 45-60 minutes of total sleep each night. That’s not just tiredness. That’s sleep deprivation with real consequences.
How Lack of Sleep Makes Pain Worse (Even When You’re Not Injured)
Here’s the part most people miss: you don’t need a new injury for pain to spike. Just one bad night of sleep can turn a dull ache into a flare-up.
Studies at Massachusetts General Hospital found that sleep loss reduces your brain’s natural pain-blocking system by 30-40%. That’s like turning down the volume on your body’s built-in painkillers. At the same time, your brain’s pain detectors-called nociceptors-get louder. You start feeling pain from things that never bothered you before, like a light touch or sitting too long.
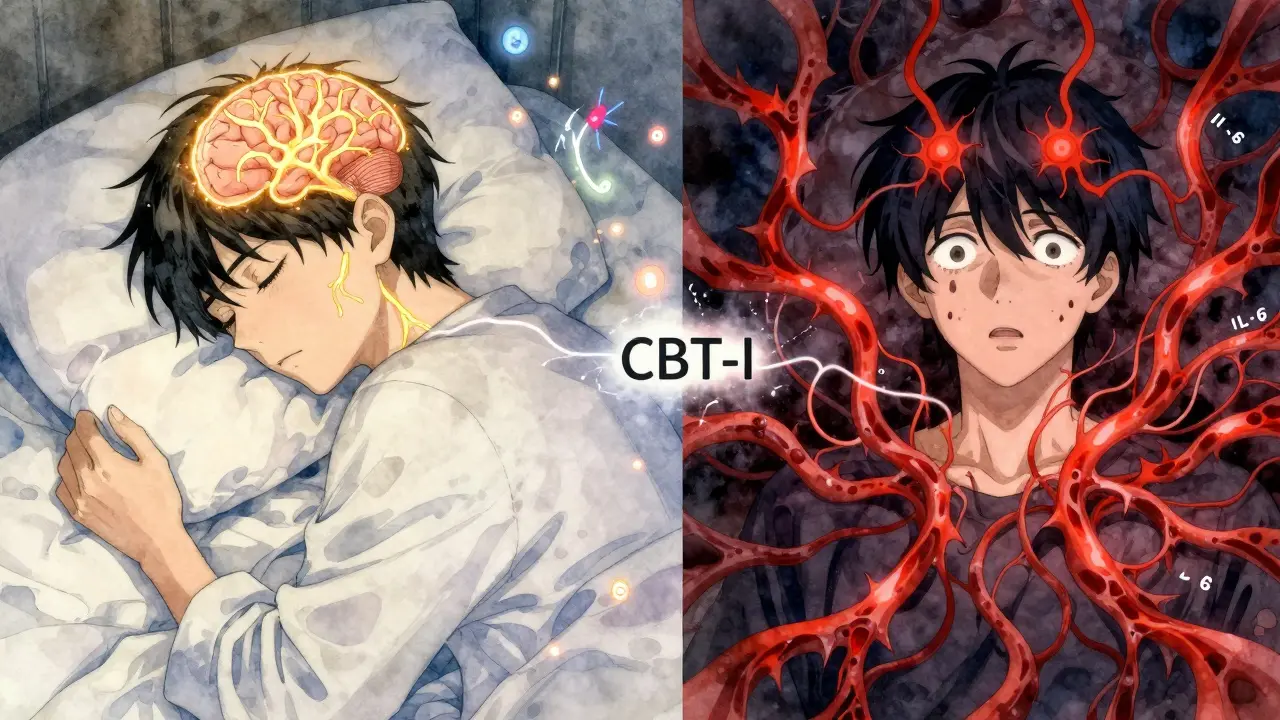
It’s not just your nerves. Your immune system goes into overdrive. Sleep deprivation increases inflammatory markers like IL-6 by 25-35%. Inflammation is a known driver of chronic pain conditions like arthritis, fibromyalgia, and lower back pain. So poor sleep doesn’t just make you hurt more-it actually makes your body produce more pain chemicals.
And then there’s dopamine. This brain chemical helps you feel reward, motivation, and yes-pain relief. After one night of bad sleep, dopamine levels drop by 20-30%. That’s why you feel hopeless, unmotivated, and more sensitive to pain the next day. It’s not in your head. It’s in your chemistry.
The Numbers Don’t Lie: Why This Cycle Is So Common
One in five adults worldwide lives with chronic pain. Of those, 50-80% report serious sleep problems. That’s over 1.5 billion people stuck in this loop.
And it’s not just about feeling tired. People with both chronic pain and insomnia report:
- 35-45% higher pain intensity
- 28% longer pain episodes
- 40% more anxiety and depression
- 50% worse ability to work, move, or enjoy life
The American Academy of Sleep Medicine says 54% of chronic pain patients meet the clinical definition of insomnia disorder. That’s more than five times the rate in the general population.
And here’s the kicker: in patient surveys, 78% say improving sleep is more important to them than reducing pain. They’re not lying. When you’re exhausted, pain feels unbearable. When you’re rested, even the same level of pain feels manageable.
Why Pain Pills and Sleep Aids Don’t Fix This
You’ve probably tried over-the-counter sleep aids. Maybe melatonin, diphenhydramine, or even prescription sleep meds. They might help you fall asleep once or twice. But they don’t break the cycle.
Here’s why:
- Most sleep aids suppress deep sleep-the most restorative stage. You sleep, but you don’t recover.
- Many pain meds, especially opioids, disrupt REM sleep and can worsen sleep apnea.
- Over-the-counter sleep aids cause next-day grogginess in 42% of users. That fog makes pain feel worse.
- They don’t address the root cause: your brain’s pain-sleep wiring.
One patient, Sarah M., shared on Reddit: “After four nights of bad sleep from back pain, my fibromyalgia goes from a 4/10 to an 8/10. It takes me two weeks to recover-even when I finally sleep.” That’s the cycle in action. Medication didn’t stop it. Sleep did.
The Only Treatment Proven to Break the Cycle: CBT-I
There’s one treatment that actually works-and it doesn’t involve pills. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I.
CBT-I isn’t just “sleep hygiene.” It’s a structured, evidence-based program that rewires how your brain thinks about sleep. It targets the thoughts and behaviors that keep you awake, even when you’re not in pain.
Here’s what happens in CBT-I for chronic pain:
- You track your sleep for two weeks-when you go to bed, how long it takes, how many times you wake up, how you feel in the morning.
- You learn to associate your bed only with sleep (no scrolling, no watching TV, no lying there worrying).
- You limit time in bed to match actual sleep time. This builds sleep pressure so you fall asleep faster.
- You reframe thoughts like “I’ll never sleep” or “If I don’t sleep, my pain will be unbearable.” These thoughts keep your brain on high alert.
- You practice relaxation techniques that calm your nervous system-not just your body, but your pain signals too.
Studies show CBT-I reduces insomnia symptoms by 65-75% in chronic pain patients. And it doesn’t stop there: it cuts pain intensity by 30-40%. That’s not a side effect. That’s the goal.
Patients who complete CBT-I gain back 12-15 percentage points in sleep efficiency. They fall asleep 25-30 minutes faster. They wake up 35-40 minutes less per night. And they report feeling more in control-of both sleep and pain.

What About New Medications? Are There Any Promising Options?
Yes-but they’re still emerging. Researchers at the University of Arizona have been studying drugs that target kappa opioid receptors, a specific pain pathway that also affects sleep. In early trials, these drugs improved sleep quality by 30-35% and reduced pain by 25-30% in people with neuropathic pain.
The FDA has given them Fast Track status, meaning they could be available within the next few years. But they’re not a magic bullet. They work best when combined with behavioral therapy.
Another promising area is personalized medicine. Scientists at Harvard have identified 12 gene variants that link pain sensitivity and sleep regulation. In the future, doctors might test your genes to predict which treatment-CBT-I, a new drug, or a combination-will work best for you.
For now, though, the most effective, accessible, and lasting solution is still CBT-I.
How to Start Breaking the Cycle Today
You don’t need to wait for a new drug or a specialist. You can start now:
- Track your sleep and pain for 10 days. Use a simple notebook or app. Note: time in bed, time asleep, pain level (1-10), and how rested you feel.
- Only go to bed when sleepy. If you’re not asleep in 20 minutes, get up. Go to another room. Read under dim light. Don’t check your phone. Come back only when sleepy.
- Keep your wake-up time fixed-even on weekends. This trains your body clock.
- Stop caffeine after 2 p.m. Even if you think it doesn’t affect you, it does.
- Get sunlight within 30 minutes of waking. Natural light resets your sleep-wake cycle better than any supplement.
- Try a free CBT-I app. Sleepio and CBT-I Coach are backed by research and work for chronic pain patients.
Don’t wait for pain to get worse. Don’t wait for your doctor to mention sleep. Start here. Right now.
Why Integrated Care Is the Future
Most pain clinics still treat pain like it’s separate from sleep. But that’s outdated. The best programs now have sleep specialists working alongside pain doctors. They use tools like the Insomnia Severity Index (ISI) to screen every patient. If your score is above 15, you get CBT-I-not just another pill.
Patients in these integrated programs report 4.7/5 satisfaction. Those in traditional pain-only clinics? 3.2/5. The difference? One treats the whole person. The other treats a symptom.
By 2023, 92% of pain clinics in the U.S. started screening for insomnia. That’s up from 35% in 2018. Change is happening. But it’s still not standard everywhere.
If your doctor doesn’t ask about your sleep, ask them. Say: “My pain is worse when I don’t sleep. Can you help me with my insomnia?”
You deserve more than a pill. You deserve rest. And rest is the missing piece in your pain management.
Can poor sleep cause chronic pain even if I didn’t have it before?
Yes. Research shows people with chronic sleep problems but no prior pain have a 56% higher risk of developing chronic pain within five years. Sleep loss lowers your pain threshold, increases inflammation, and weakens your brain’s natural pain-blocking systems. Over time, this can trigger conditions like fibromyalgia, back pain, or headaches-even without injury.
Is CBT-I effective for people with severe pain?
Yes. Studies show CBT-I works just as well for people with severe chronic pain as it does for those with mild pain. It doesn’t eliminate pain, but it reduces how much it affects your sleep-and that’s what breaks the cycle. Patients report less pain intensity, not because the injury changed, but because their brain stopped overreacting to it.
How long does it take for CBT-I to reduce pain?
Most people see improvements in sleep within 2-3 weeks. Pain reduction usually follows after 4-6 weeks. By week 8-10, patients report 30-40% less pain intensity on average. The key is consistency-skipping sessions slows progress.
Can I do CBT-I on my own, or do I need a therapist?
You can start with digital programs like Sleepio or CBT-I Coach, which have 60-65% success rates in chronic pain patients. But working with a certified CBT-I therapist increases success to 75% and improves long-term results. If you’re struggling with anxiety, depression, or complex pain, a therapist is strongly recommended.
What if I can’t fall asleep even after trying CBT-I?
It’s normal to have setbacks. CBT-I isn’t about forcing sleep-it’s about removing the barriers to it. If you’re still struggling after 8-10 weeks, talk to a sleep specialist. You might have an underlying condition like sleep apnea or restless legs syndrome. These are treatable, and fixing them can unlock better sleep.
Comments (14)
-
kelly tracy December 30, 2025
Let me guess - you’re one of those people who thinks CBT-I is some magical cure-all while ignoring the fact that 70% of chronic pain patients can’t even afford to see a therapist, let alone spend 8 weeks on an app. Your entire post reads like a pharmaceutical industry sales pitch disguised as science. Wake up. Not everyone has the luxury of time, energy, or money to ‘track their sleep.’ Some of us are working two jobs and sleeping in 20-minute chunks between shifts. Stop pretending this is a simple fix.
-
srishti Jain December 31, 2025
CBT-I? More like CBT-WhyAmINotSleepingYet. I tried it. Woke up at 3am thinking about my pain, then thought about how I’m thinking about my pain, then thought about how I’m overthinking it. Ended up crying into my pillow. No magic. Just more exhaustion.
-
Cheyenne Sims January 1, 2026
The grammatical errors in your article are unacceptable. ‘You’re not broken’ is a colloquialism, not a medical statement. The misuse of ‘it’s’ versus ‘its’ in paragraph three is egregious. Furthermore, the claim that ‘sleep deprivation increases IL-6 by 25-35%’ lacks proper citation. This is not science - it’s pseudoscientific clickbait dressed in academic formatting. I expect better from a platform that purports to inform.
-
Glendon Cone January 2, 2026
Bro. I’ve been in this cycle for 7 years. Back pain + insomnia = living in a nightmare. I tried everything - melatonin, opioids, yoga, cryotherapy, even a $1,200 mattress. Nothing worked until I did CBT-I through a VA app. Not overnight. But after 5 weeks? I slept 5 hours straight for the first time in years. My pain didn’t vanish… but it stopped screaming. I’m not crying about it anymore. Just grateful. 🙏
-
Henry Ward January 3, 2026
Oh wow, another ‘sleep is the real cure’ guru. Let me guess - you’ve never had a herniated disc or neuropathy. You think if you just ‘reprogram your brain,’ your sciatica will magically disappear? Wake up. Pain isn’t a mindset. It’s biology. And when your nerve is pinched, no amount of sleep hygiene is going to fix a bulging disc. This post is dangerously naive. People are suffering, not philosophizing.
-
Aayush Khandelwal January 5, 2026
Let’s not reduce this to binary solutions - CBT-I vs pills. The neuroplasticity angle here is fascinating. Pain and sleep are co-regulated via the limbic-thalamocortical loop. When you disrupt sleep architecture, you dysregulate the descending inhibitory pathways - think PAG-RVM axis. CBT-I doesn’t ‘fix’ pain; it recalibrates the gain control on nociceptive signaling. That’s why pain drops - not because the injury healed, but because the CNS stopped overamplifying. We need more of this systems-level thinking in clinical practice.
-
Sandeep Mishra January 6, 2026
Hey, I know how heavy this feels. Been there - 10 years with fibro, 5 years of sleepless nights. I didn’t believe in CBT-I either. Thought it was ‘just meditation.’ But I did the 8-week program with a therapist who actually understood chronic pain. It didn’t erase the pain. But it gave me back my nights. And that’s everything. You’re not weak for needing help. You’re brave for even reading this. Take it slow. One breath. One night. You’ve got this.
-
Joseph Corry January 6, 2026
How quaint. You’ve reduced a complex neurobiological phenomenon - the bidirectional modulation of nociception and sleep architecture - to a self-help checklist. CBT-I, sunlight, caffeine cutoffs… as if the human nervous system is a poorly calibrated thermostat. The real issue? Capitalist healthcare commodifies ‘solutions’ like this, turning suffering into a productized behavioral intervention. Meanwhile, the systemic failures - lack of access, insurance denials, pharmaceutical lobbying - remain untouched. You’re not healing anyone. You’re selling a myth.
-
Colin L January 7, 2026
Look, I’ve been through this. I’ve had spinal fusion, failed epidurals, and spent 14 months on opioids that made me feel like a zombie. I tried CBT-I. It helped a little. But here’s the thing no one talks about - the loneliness. You lie there at 3 a.m., your body screaming, your mind racing, and you realize no one really gets it. Not your partner, not your doctor, not even your therapist. They say ‘sleep better’ like it’s a switch. But it’s not. It’s a war inside your own skin. And you’re fighting it alone. I just wanted someone to say - I see you. Not fix you. Just see you.
-
Hayley Ash January 8, 2026
Oh so now sleep is the magic wand? Next you’ll tell me to hug a tree and visualize my pain dissolving. I’ve got arthritis in my hips, not a bad attitude. Your entire post reads like a wellness influencer’s dream. Congrats. You’ve turned chronic pain into a productivity hack. Bravo. 🙃
-
Shae Chapman January 8, 2026
I cried reading this. Not because it’s perfect - but because for the first time, someone actually described what it’s like. I’ve been told ‘it’s all in your head’ so many times I stopped believing my own body. CBT-I didn’t fix my pain. But it gave me back my nights. And that’s the difference between surviving and living. Thank you. I’m signing up for Sleepio today. 💙
-
Nadia Spira January 9, 2026
CBT-I? Please. You’re just repackaging placebo with jargon. If sleep were the solution, everyone with insomnia would be pain-free. But they’re not. You’re ignoring the structural causes - inflammation, autoimmunity, environmental toxins. And you’re blaming the patient for not being disciplined enough. This isn’t healing. It’s victim-blaming with a PhD.
-
henry mateo January 10, 2026
hey i just wanted to say i tried the cbt-i coach app and it actually helped me sleep better even though my pain is still there. i didnt think it would work but i kept at it and now i dont panic when i wake up at 3am anymore. thank you for writing this. also sorry for typos im typing on my phone and my hands hurt
-
Kunal Karakoti January 10, 2026
The real question isn’t whether CBT-I works - it’s whether we’re willing to accept that pain is not a problem to be solved, but a signal to be understood. We’ve built a medical system that treats discomfort as an enemy to be eradicated. But what if pain, like grief, is part of being human? What if the goal isn’t to eliminate it, but to live beside it with grace? Sleep is not the cure. It’s the space where we learn to listen.
