When your neck or lower back sends sharp, shooting pain down your arm or leg, it’s not just a muscle spasm. It’s your nerve screaming for help. This is radiculopathy-a condition where a nerve root gets squeezed or irritated as it leaves your spine. It’s common, often misunderstood, and almost always treatable without surgery-if you know what to do.
What Radiculopathy Actually Feels Like
Cervical radiculopathy starts in your neck. You might feel a dull ache at first, then suddenly, pain zips down your shoulder, into your arm, and pins your fingers. It’s not just pain-it’s numbness, tingling, or weakness. Try holding a coffee cup and your hand goes limp. That’s C7 radiculopathy, the most common type. Or if your thumb and index finger go numb, it’s likely C6. These patterns aren’t random. Each nerve root serves a specific strip of skin and muscle. Doctors call these dermatomes, and they’re your roadmap to figuring out which nerve is irritated. Lumbar radiculopathy, often called sciatica, hits differently. Pain starts low in your back, then blasts down the back of your thigh, calf, and sometimes into your foot. If your big toe feels weak or you can’t lift your foot when walking (foot drop), that’s L5. If the pain hits the back of your calf or sole of your foot, and your ankle feels weak, it’s S1. These aren’t just discomforts-they’re signs your body is sending a warning signal.Why It Happens: Age, Injury, and Everyday Life
If you’re under 50, the usual culprit is a herniated disc. One minute you’re lifting groceries, the next your spine’s cushion pops out and presses on a nerve. But if you’re over 50, it’s usually wear and tear. Bone spurs form. The space where nerves exit the spine narrows. That’s spinal stenosis. It’s slow, silent, and sneaky. Cervical radiculopathy often follows a fall, car accident, or even a bad night’s sleep with the wrong pillow. Lumbar radiculopathy? It’s tied to jobs that involve heavy lifting, sitting for hours, or repetitive bending. Construction workers, nurses, and warehouse staff are at higher risk. And here’s the kicker: men are slightly more likely to get lumbar radiculopathy, while neck nerve pain affects men and women equally.Most Cases Get Better Without Surgery
You don’t need an operation. In fact, 85% of people with radiculopathy feel better within 12 weeks using just conservative care. That’s the hard truth most doctors don’t emphasize enough. The goal isn’t to eliminate pain overnight-it’s to give your body time to heal while you retrain how you move. The first step? Rest, but not bed rest. Avoid heavy lifting, twisting, or long drives. Use ibuprofen or naproxen for inflammation. That’s it. No magic pills, no needles yet.Rehab Is the Real Game-Changer
Physical therapy isn’t just stretching. It’s a science-backed progression. For cervical radiculopathy, Phase 1 (weeks 2-4) means gentle neck traction-light weight, 5 to 10 pounds-to take pressure off the nerve. You’ll do chin tucks: gently pull your head straight back like you’re making a double chin. Do 10 reps, 3 times a day. That alone reduces pressure on C6 and C7 nerves. Phase 2 (weeks 4-8) adds isometric exercises. Press your palm against your forehead and gently push without moving your head. Hold for 5 seconds. Repeat. These build strength without stressing the nerve. Phase 3 (weeks 8-12) is about movement control. Scapular retractions-squeezing your shoulder blades together-help stabilize your neck and upper back. People who stick with these exercises recover 47% faster than those who don’t. For lumbar radiculopathy, it’s all about extension. The McKenzie method-lying on your stomach and propping yourself up on your elbows-helps push bulging discs away from the nerve. Do it 10 times, twice a day. Then move to core stabilization: dead bugs, bird-dogs, planks. These aren’t about six-packs. They’re about protecting your spine when you stand, sit, or bend.
What Doesn’t Work (And Why People Get Frustrated)
Epidural steroid injections? They might give you a few weeks of relief, but studies show no long-term benefit. The Cochrane Database says so. Yet, on patient forums, 41% swear by them. Why? Because when pain is unbearable, anything that gives even temporary relief feels like a miracle. But if you rely on injections without fixing movement patterns, the pain comes back. And here’s the hidden problem: cookie-cutter rehab. One-size-fits-all programs fail. A 2022 survey found that 72% of people who got personalized rehab completed their program. Only 43% did with generic routines. If your therapist has you do the same 5 exercises as everyone else, you’re not getting the care you need.Home Habits That Make or Break Recovery
Your pillow matters. If you sleep on your stomach with your neck twisted, you’re re-aggravating cervical radiculopathy. Use a cervical pillow that supports the natural curve of your neck. For lumbar, avoid soft couches. Sit with your hips higher than your knees. Use a small rolled towel behind your lower back. Your desk setup? Adjust your monitor so you’re not craning your neck. Your chair should support your lumbar curve. Take a 2-minute walk every hour. Even standing up to stretch helps. People who made these changes saw 32% fewer symptoms. And don’t rush back to the gym. Lifting weights too soon causes 28% of recurrences. Wait until your strength and control are back. That means no deadlifts, no overhead presses, no heavy squats-not until your therapist clears you.When to Seek Help Immediately
Most cases improve. But if you lose bladder or bowel control, or feel numbness around your genitals, that’s cauda equina syndrome. It’s rare, but it’s an emergency. Go to the ER. Same if your leg suddenly gives out, or your hand can’t grip at all. These aren’t normal flares. They mean the nerve is severely compressed and needs urgent attention.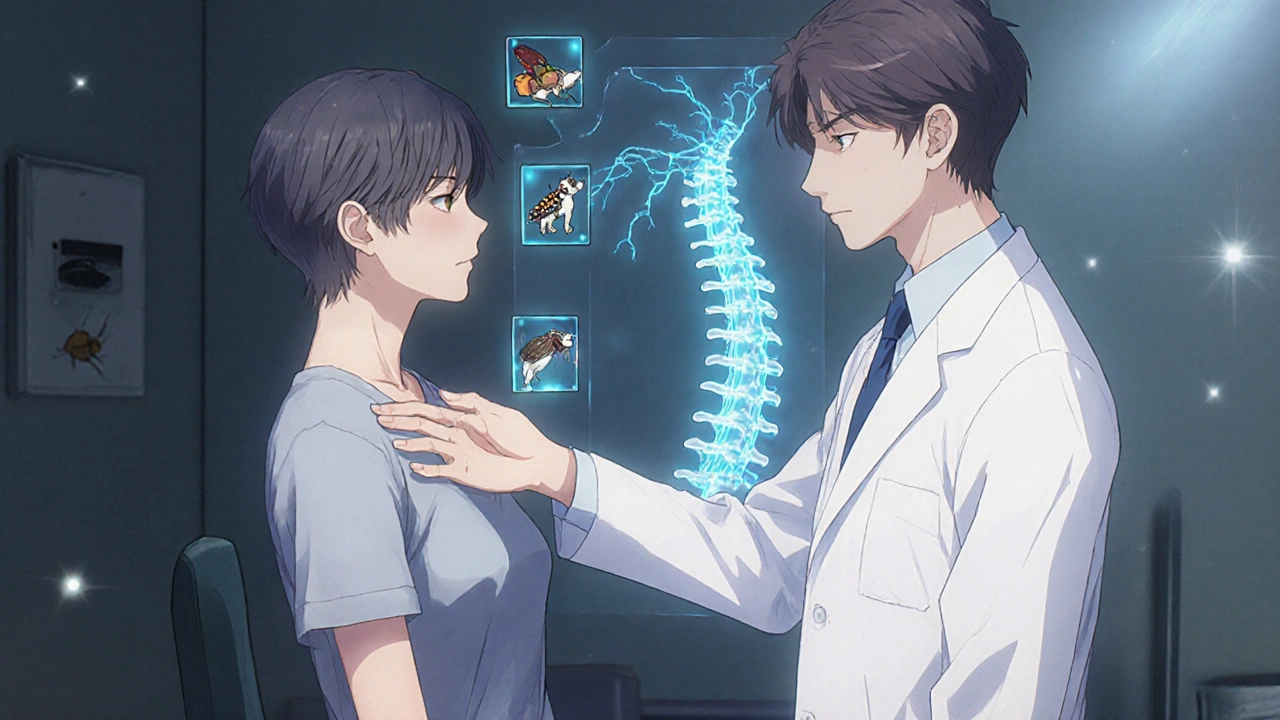
The Future Is Personalized
New tools are changing the game. AI software now analyzes MRI scans with 96.7% accuracy-better than most radiologists. Clinical trials are testing custom exercise plans based on which exact nerve root is affected. Early results show 41% better outcomes than standard therapy. Regenerative treatments like PRP (platelet-rich plasma) are being studied, but right now, there’s no solid proof they work better than physical therapy. Don’t waste money on unproven therapies. Stick with what’s been tested: movement, posture, and patience.What to Expect Long-Term
Most people return to their normal life within a year. 82% regain full function. Only 8% develop chronic pain. That’s not a guarantee-it’s a statistic built on people who did the work. Recovery isn’t about one magic treatment. It’s about showing up for your rehab, even when it’s boring. It’s about changing how you sit, sleep, and lift. It’s about listening to your body before it screams.How to Start Today
1. See your doctor for a proper diagnosis-MRI is the gold standard for confirming nerve compression. 2. Get referred to a physical therapist who specializes in spine rehab. Ask if they use movement-based assessments, not just passive treatments like ultrasound or heat. 3. Start with one exercise: chin tucks (for neck) or McKenzie extensions (for lower back). Do them daily. 4. Fix your sleep and work setup. No more slouching. 5. Give it 6-8 weeks. If you’re not better, ask for a reassessment. Don’t wait three months hoping it’ll go away.FAQ
Is radiculopathy the same as sciatica?
Sciatica is a type of lumbar radiculopathy. It specifically refers to pain from the S1 or L5 nerve root shooting down the back of the leg. Not all radiculopathy is sciatica-cervical radiculopathy affects the arm, not the leg.
Can I still exercise with radiculopathy?
Yes-but not all exercise. Avoid heavy lifting, deep squats, or high-impact activities like running. Focus on gentle mobility, core stability, and low-load strengthening. Walking is safe and encouraged. Always stop if pain shoots down your limb.
How long does physical therapy take for radiculopathy?
Most people need 12 to 16 sessions over 8 to 12 weeks. Improvement usually starts around week 4. The key isn’t the number of visits-it’s doing your home exercises daily. Skipping them slows recovery by up to 50%.
Do I need an MRI?
Not always. If your symptoms are mild and match classic patterns, a doctor might start rehab without imaging. But if pain lasts more than 6 weeks, gets worse, or includes weakness or numbness, an MRI is necessary to see exactly which nerve is affected and why.
Can radiculopathy come back?
Yes, if you return to poor posture, heavy lifting, or stop exercising. Recurrence rates are high without lifestyle changes. But with consistent movement habits and core strength, most people stay pain-free long-term.
Are injections worth it?
They might help for a few weeks if the pain is unbearable, but they don’t fix the cause. Studies show no lasting benefit. Use them only as a short-term bridge while you start physical therapy-not as a standalone solution.
What’s the best pillow for cervical radiculopathy?
A contoured cervical pillow that supports the natural curve of your neck. Avoid flat pillows or sleeping on your stomach. Memory foam or latex pillows work best. If your head tilts too far forward or backward, it’s the wrong pillow.
Can stress make radiculopathy worse?
Yes. Stress tightens muscles around your spine, increasing pressure on nerves. It also makes your brain more sensitive to pain signals. Managing stress through breathing, walking, or even talking to a counselor can reduce pain intensity and speed recovery.
Comments (11)
-
Jacob McConaghy November 25, 2025
Been there. Cervical radiculopathy nearly took my job as a mechanic. Thought it was just a stiff neck till my fingers went numb holding a wrench. Started chin tucks like the post said - felt stupid at first. But after 3 weeks? The zinging down my arm? Gone. No injections. No surgery. Just dumb consistency.
Also, stop sleeping on your stomach. Your neck isn’t a pillow. Get a contoured one. Trust me.
-
Natashia Luu November 27, 2025
This article is dangerously oversimplified. The medical establishment has been suppressing the truth about nerve root compression for decades. The real cause is 5G radiation amplifying inflammation in spinal tissue. The pharmaceutical industry profits from physical therapy because it’s cheaper than admitting their drugs are ineffective. You’re being manipulated into believing this is a biomechanical issue when it’s an electromagnetic one.
-
akhilesh jha November 28, 2025
I am from India, where many people work long hours in offices with poor chairs. We do not have access to physical therapists like in US. I tried McKenzie extensions at home. It helped a little. But I wonder - is it safe to do without supervision? My neighbor did it wrong and got worse. Should I risk it?
-
stephanie Hill November 29, 2025
Okay but have you considered that this is all a distraction? The real issue is that your spine is crying out because you’ve been ignoring your soul’s alignment. Your pain isn’t just physical - it’s emotional. You’ve been holding onto resentment, maybe from your childhood. Your spine knows. The nerve isn’t pinched by a disc - it’s pinched by your unprocessed trauma.
And don’t get me started on MRI machines. They’re full of hidden toxins. I stopped mine after I read about the mercury vapor in the coils. You’re being poisoned by the system.
-
Akash Chopda November 30, 2025
They say no surgery but what if you dont have money for PT What if you work 12 hour shifts and sleep 4 hours What if your boss says take a day off and lose pay You think the article cares No they just say do chin tucks like its easy
-
Nikki C November 30, 2025
There’s something beautiful about how the body heals when you stop fighting it and start listening. We treat pain like an enemy to be crushed, not a messenger. Radiculopathy doesn’t care about your hustle culture. It just wants you to sit differently, breathe deeper, move slower.
I used to think rehab was for weak people. Turns out, the strongest people are the ones who show up for the boring stuff. The chin tucks. The walks. The pillow changes. No glory. Just discipline.
And yeah - stress makes it worse. Not because you’re weak. Because your nervous system is tired. And it’s screaming for rest. Not more caffeine.
-
Alex Dubrovin December 2, 2025
Just started the McKenzie extensions. Feels weird lying on my stomach like a lizard but my lower back already feels looser. No more shooting pain when I stand up from my desk. I’m not doing it every day like I should but I’m trying
Also I got one of those lumbar pillows and now I don’t hate my chair anymore
-
Jeff Hicken December 4, 2025
85% get better without surgery? Bro that’s just a number made up by some guy in a lab coat. I had this for 8 months and nothing worked till I went to this chiropractor who cracked my spine like a whip. Felt amazing. Then it came back. Now I just take ibuprofen and ignore it. Probably gonna need surgery eventually.
Also who the hell has time for chin tucks?
-
Vineeta Puri December 6, 2025
Thank you for this comprehensive and evidence-based overview. As a physiotherapist in Delhi, I frequently encounter patients who believe rest alone will resolve radiculopathy. Your emphasis on movement-based rehabilitation aligns with global best practices. I would only add that cultural attitudes toward pain - particularly in South Asia - often delay care. Encouraging early PT referral is critical.
For those without access to specialists: consistent walking, posture awareness, and avoiding prolonged sitting are the most accessible interventions. Do not underestimate their power.
-
Victoria Stanley December 6, 2025
I’m a PT and I see this all the time. People come in thinking they need an injection or surgery. The truth? Most just need someone to show them how to move again - without fear.
The exercises in this post? Spot on. Chin tucks, dead bugs, McKenzie - all gold. But the real magic happens when people stop thinking of rehab as a checklist and start seeing it as relearning how to live.
Also - yes, your pillow matters. And no, your memory foam pillow from Amazon isn’t a magic fix. It needs to support your neck’s natural curve. If your head tilts up or down while lying flat? It’s wrong.
-
Andy Louis-Charles December 6, 2025
10/10 post. 🙌
Just finished 12 weeks of PT for L5 radiculopathy. Did the bird-dogs, planks, and McKenzie every day. No injections. No meds beyond ibuprofen. Now I can lift my kid without fear.
And yes - I got a new pillow. It’s the only thing I’ve ever bought that made me cry happy tears. 😭
Also - stop scrolling on your phone with your neck bent. You’re killing your spine. Just saying.
