
Every year, Americans spend over $700 billion on prescription drugs. But here’s the catch: generic drugs make up 90% of all prescriptions filled - yet they cost just 12% of that total. That’s not a fluke. It’s the single biggest reason the U.S. healthcare system hasn’t collapsed under the weight of drug prices.
How Generics Save $482 Billion a Year
In 2024, Americans filled 3.9 billion prescriptions for generic medications. That’s 9 out of every 10 pills taken. Yet those generics only cost $98 billion. Meanwhile, brand-name drugs - just 10% of prescriptions - sucked up $700 billion. The difference? $482 billion in savings. That’s more than the entire annual budget of the Department of Education.
This isn’t new. Since 2016, generics have consistently covered 90% of prescriptions while their share of spending dropped from 27% to 12%. That means even as more people use generics, the cost per pill keeps falling. Why? Because once a patent expires, multiple manufacturers can make the same drug. Competition drives prices down - sometimes by 80% to 95%.
Take albuterol, the asthma inhaler. The brand version costs over $60 per inhaler. The generic? Around $20. For someone using it daily, that’s a $300 monthly savings. One Reddit user shared that switching to generic albuterol cut their out-of-pocket cost by 85%. That’s the kind of relief that keeps people alive - and out of emergency rooms.
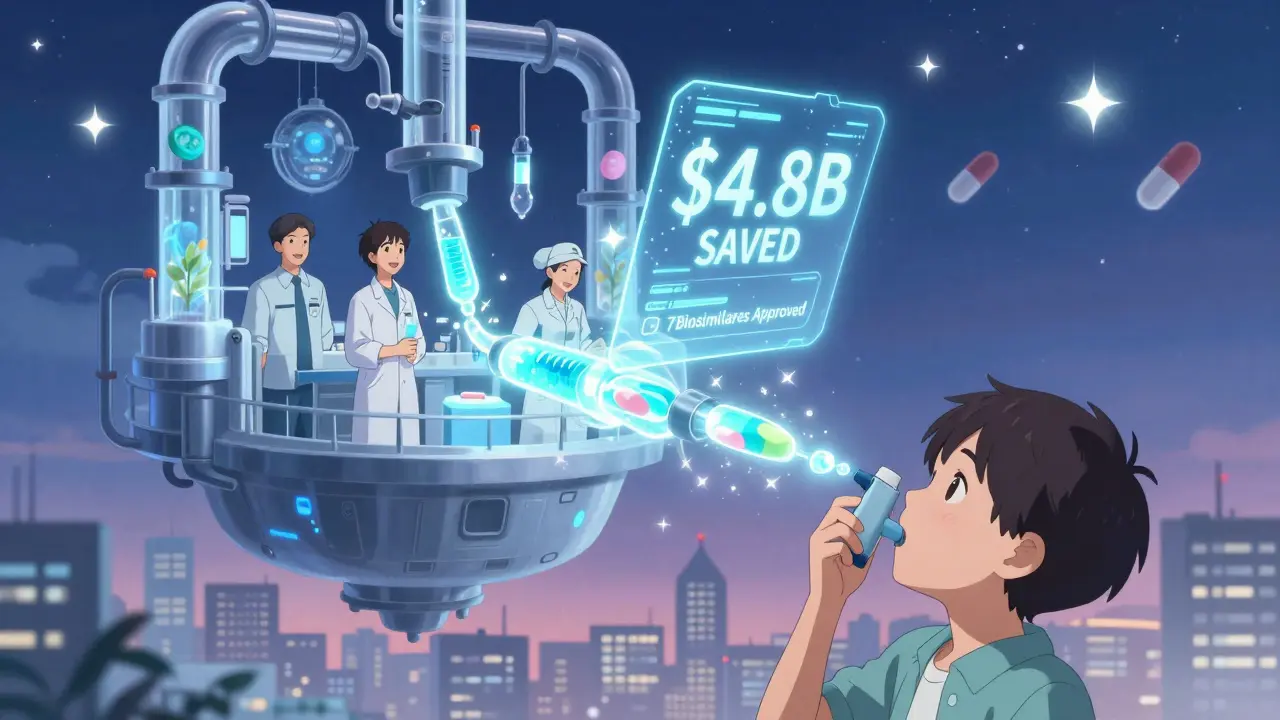
Biosimilars: The Next Wave of Savings
Generics aren’t the whole story. Biosimilars - cheaper versions of complex biologic drugs like Humira, Enbrel, and Stelara - are now hitting the market. These aren’t simple pills. They’re made from living cells, so copying them is harder. But they still cost 80% less than the original.
In 2024, Humira biosimilars went from 3% market share to 28% after health plans started pushing them. That single shift saved billions. Now, Stelara - a $6 billion drug - has seven biosimilars approved. Once fully adopted, they’re projected to save $4.8 billion a year.
Since 2015, biosimilars have enabled over 460 million extra days of patient therapy. That’s hundreds of thousands of people who could’ve gone without treatment if prices stayed high. But here’s the problem: 90% of biologics losing patent protection in the next 10 years have zero biosimilars in development. That’s a $234 billion missed opportunity.
Why Brand Drugs Cost So Much
Why do brand-name drugs cost three times more in the U.S. than in other wealthy countries? It’s not because they’re better. It’s because the system lets them.
Big pharma uses legal tricks to delay generics. One common tactic is "pay for delay" - where the brand-name company pays a generic maker to stay off the market. In 2024, these deals cost an average of $1.2 billion per year in settlements. That’s money spent to keep prices high, not to develop new drugs.
Another issue? Patents. Some companies file dozens of minor patents on a single drug - for packaging, dosage forms, or delivery methods - just to extend exclusivity. This is called "evergreening." It’s legal, but it blocks competition for years.
Compare that to insulin. In 2023, Eli Lilly’s insulin cost $275 per vial. After public pressure and Medicare negotiations, they dropped it to $25. That’s not because the drug changed. It’s because someone finally pushed back.

How Medicare and Policy Are Changing the Game
The Inflation Reduction Act gave Medicare the power to negotiate prices for 10 drugs in 2026, rising to 30 by 2029. The Congressional Budget Office estimates this could save $500-550 billion over 10 years. If those same rules applied to Medicaid and private insurance? Savings could top $1 trillion.
Already, Medicare beneficiaries pay no more than $35 per month for insulin in 2025. That cap expands to commercial plans by 2027. That’s huge. Before, seniors hitting the catastrophic coverage phase often used only brand-name drugs because generics weren’t enough to cover their costs. Now, they’re switching to generics - and saving thousands.
White House deals with Eli Lilly and Novo Nordisk have also cut Ozempic and Wegovy prices from over $1,000 to $350 per month. These aren’t generics. But they show what happens when the government steps in. The same pressure could force brand-name companies to lower prices - or risk losing market share to generics.
Who’s Really Paying the Price?
It’s not just the system. It’s people.
GoodRx found that nearly 1 in 12 Americans has medical debt because of prescription costs. For many, the choice isn’t between two drugs - it’s between buying medicine and paying rent. A 68-year-old with diabetes might skip doses because their $400 monthly insulin bill eats up their Social Security check. A parent with asthma might ration their inhaler because the generic they need isn’t covered by their plan.
Pharmacists often swap one generic for another. That’s called a therapeutic interchange. But not all generics are the same. Some have different fillers or release rates. One patient reported switching from one generic metformin to another and developed severe stomach pain. The drug worked - but the side effects didn’t. That’s why some doctors still prefer brand-name drugs. But that’s a cost burden on patients.
The Bigger Picture: Savings That Keep the System Alive
Prescription drugs account for 10.3% of all U.S. healthcare spending. Without generics, that number would be close to 25%. The entire system depends on them.
The generic industry supports 350,000 jobs across 46 states. It’s not just pills on a shelf - it’s factories, labs, logistics, and pharmacists. But the industry is under pressure. In 2024, the FDA issued 1,247 inspection violations for manufacturing quality issues. That’s a red flag. If quality slips, trust slips. And if trust slips, patients stop using generics - even if they’re cheaper.
By 2030, experts predict generic and biosimilar use could reduce total U.S. drug spending by 15-18%. That’s $100-120 billion in annual savings. But only if we fix the roadblocks: pay-for-delay deals, lack of biosimilar development, and insurance barriers.
What Needs to Change
Three things are critical:
- End pay-for-delay deals. These are anti-competitive and illegal under antitrust law - but enforcement is weak. Congress needs to ban them outright.
- Speed up biosimilar approvals. The FDA needs more funding and staff to review biosimilar applications faster. Right now, it takes years.
- Expand price negotiation. Medicare’s power should extend to all payers. Private insurers should be required to cover generics and biosimilars at the lowest possible price.
Health plans can help too. They need to stop penalizing biosimilars with high copays. They need to simplify prior authorizations. And they need to pay pharmacists fairly for switching patients to cheaper alternatives.
At the end of the day, generic drugs aren’t a niche option. They’re the backbone of affordable care. Without them, millions would go without treatment. Without them, the U.S. healthcare system would be unaffordable for everyone - not just the uninsured.
The data doesn’t lie. Generics save lives. They save money. And they’re the most effective tool we have to fix a broken drug pricing system. The question isn’t whether we can afford more generics. It’s whether we can afford not to use them.
Comments (15)
-
Alex Warden January 2, 2026
Let me tell you something straight - if you think generics are the whole solution, you’re sleeping on the real problem: Big Pharma owns Congress. Pay-for-delay? That’s not a loophole - it’s a bribe with a law degree. And don’t even get me started on how insurance companies still make you pay $50 for a generic because they got a kickback from the brand. This isn’t about savings - it’s about power.
-
jaspreet sandhu January 3, 2026
in india we pay like 5 dollars for same medicine that cost 50 in usa. why? because here no one cares about patent. company make it and sell it. no lawsuit. no delay. no 1000 page paperwork. people live. people get better. in usa you need a lawyer to buy aspirin. this is not healthcare. this is a casino with stethoscopes.
-
LIZETH DE PACHECO January 5, 2026
I’ve seen patients cry because they had to choose between insulin and groceries. Generics aren’t just numbers on a spreadsheet - they’re dignity. I work in a clinic, and when we switch someone to a generic that works, it’s not just cheaper - it’s life-changing. We need more pharmacists paid to help with those switches, not penalized for it.
-
Lee M January 5, 2026
Here’s the truth nobody wants to admit: capitalism doesn’t care if you die. The system isn’t broken - it’s working exactly as designed. Profit over people. Patent trolling is the new feudalism. And the FDA? A rubber stamp for corporate lobbyists. We don’t need more studies. We need a revolution.
-
Bryan Anderson January 7, 2026
The data on generic adoption is overwhelmingly positive, and the cost savings are well-documented. However, we must also acknowledge that some patients experience variability in therapeutic response due to differences in inactive ingredients. While this is rare, it’s not negligible. A more nuanced approach to formulary management - including pharmacist-led therapeutic substitution protocols - could reduce adverse events while preserving savings.
-
Matthew Hekmatniaz January 9, 2026
I grew up in a country where medicine was a human right, not a commodity. Coming to the U.S. was a shock. I didn’t understand why someone would skip their meds because they couldn’t afford the $35 copay on a generic. It’s not about patriotism. It’s about basic decency. We can do better - and we have the tools. We just need the will.
-
Liam George January 9, 2026
Ever wonder why the FDA approves generics so fast but blocks biosimilars for years? Coincidence? Or is this part of the Great Pharma Cover-Up? The same people who told you vaccines were dangerous are now pushing ‘biosimilar safety’ - funded by the same donors. They don’t want you to know that generics are actually safer - cheaper, yes, but also more regulated because they’re mass-produced. Trust the system? Nah. Trust your gut.
-
sharad vyas January 10, 2026
in india we grow the plants for many of these medicines. our farmers and labs make the raw stuff. then american companies buy it, put it in a fancy bottle, slap a patent on it, and sell it back to us for ten times more. this is not trade. this is colonialism with a pharmacy license. we make the medicine. you make the profit. and we still pay more for it.
-
Dusty Weeks January 11, 2026
generics are fine i guess 🤷♂️ but like... what if the brand name one just works better? 😔 i mean i saw a guy on tiktok say his generic Adderall made him feel like a zombie. like... who even knows anymore?? 💊😭
-
Sally Denham-Vaughan January 12, 2026
My grandma switched to generic metformin last year. No side effects. Saved her $200/month. She said, ‘Honey, I didn’t know medicine could be this simple.’ That’s the real story here. Not the politics. Not the patents. Just a woman who can now afford to live. Sometimes the simplest solution is the most powerful one.
-
Bill Medley January 14, 2026
Generic drugs are a net positive for public health and fiscal sustainability. Policy interventions must prioritize market access, regulatory efficiency, and equitable reimbursement structures to maximize impact.
-
Ann Romine January 15, 2026
I’ve worked in pharmacy for 22 years. I’ve seen generics go from being seen as ‘cheap alternatives’ to being the only option many patients can afford. But I’ve also seen the confusion - patients think ‘generic’ means ‘weaker.’ It’s not about the drug. It’s about the story we tell. We need to change the narrative, not just the price tag.
-
Todd Nickel January 16, 2026
It’s fascinating how the same people who scream about government overreach are perfectly fine with pharmaceutical monopolies that cost billions in lost productivity and preventable ER visits. The market isn’t free - it’s rigged. And the people who suffer aren’t the CEOs. They’re the ones holding two prescriptions, trying to decide which one to skip this month. The math is simple: 90% of prescriptions are generic. That’s not a trend. That’s a rebellion.
-
Austin Mac-Anabraba January 18, 2026
Let’s be brutally honest: generics are the only reason the U.S. hasn’t imploded from healthcare costs. But don’t pretend this is altruism. It’s desperation. The system is so broken that even Big Pharma knows they can’t keep charging $1000 for a pill forever. So they quietly let generics in - but only after squeezing every last dime out of the brand version. This isn’t progress. It’s damage control.
-
Phoebe McKenzie January 19, 2026
YOU THINK THIS IS ABOUT MONEY? NO. IT’S ABOUT CONTROL. THEY WANT YOU TO BE DEPENDENT. THEY WANT YOU TO BELIEVE YOU NEED THEIR BRAND. THEY WANT YOU TO BE AFRAID OF THE GENERIC. THEY WANT YOU TO PAY MORE. THEY WANT YOU TO BE STUPID. AND THEY’RE WINNING. 😡
