
Secondary Hypogonadism & Chronic Fatigue Risk Calculator
Enter your symptoms and hormone levels, then click "Calculate Risk" to see if secondary hypogonadism may be contributing to your fatigue.
Did you know that up to 30% of men who report relentless exhaustion actually have a hidden hormone problem? Secondary hypogonadism can be the missing link behind chronic fatigue, and understanding the connection can change how you feel day to day.
TL;DR
- Secondary hypogonadism is a pituitary‑driven drop in testosterone, not a testicular issue.
- Low testosterone reduces energy, muscle mass, and mood, often masquerading as chronic fatigue.
- Key clues: reduced libido, morning weakness, low LH/FSH, and normal testicular size.
- Blood tests (total & free testosterone, LH, FSH) confirm the diagnosis.
- Treatment includes testosterone therapy, pituitary‑targeted meds, and lifestyle tweaks.
What Is Secondary Hypogonadism?
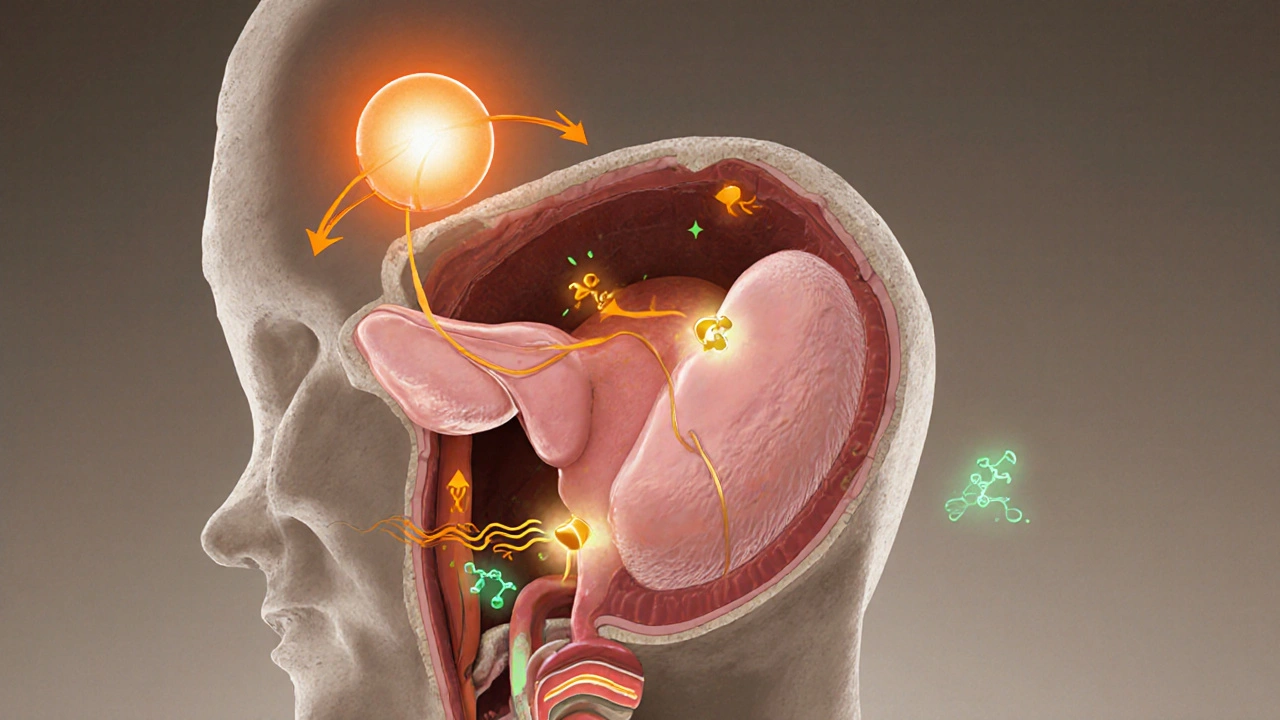
Secondary hypogonadism is a condition where the pituitary gland fails to signal the testes to produce adequate testosterone. Unlike primary hypogonadism, the testes themselves are usually normal; the problem lies upstream in the hypothalamic‑pituitary‑gonadal (HPG) axis.
The pituitary releases two key hormones: luteinizing hormone (LH) and follicle‑stimulating hormone (FSH). When LH and FSH are low, testosterone production drops, leading to a cascade of symptoms.
Why Does It Matter for Energy Levels?
Testosterone isn’t just about muscle and libido; it’s a metabolic regulator. It influences metabolic rate, mitochondrial efficiency, and even the quality of sleep architecture. When levels dip, you often feel a “brain fog” that overlaps heavily with the hallmark signs of chronic fatigue.
Research from the Endocrine Society (2023) showed that men with testosterone < 300 ng/dL reported a 45% increase in daytime sleepiness scores compared to age‑matched controls.
Chronic Fatigue: More Than Just Tiredness
Chronic fatigue (often labeled as chronic fatigue syndrome or myalgic encephalomyelitis) is defined by persistent, unexplained exhaustion lasting at least six months, unrelieved by rest.
Symptoms span physical and mental realms: post‑exertional malaise, unrefreshing sleep, joint pain, and cognitive impairment. Because the diagnostic criteria are symptom‑based, hormone deficiencies frequently slip under the radar.
How Secondary Hypogonadism Triggers Fatigue
- Reduced Muscle Power: Lower testosterone shrinks fast‑twitch fibers, so everyday tasks feel harder.
- Impaired Mood Regulation: Testosterone modulates serotonin and dopamine pathways; deficiency can lead to depression, which amplifies perceived fatigue.
- Sleep Disruption: Men with secondary hypogonadism often experience lighter sleep stages, waking up feeling unrested.
- Metabolic Slow‑down: Basal metabolic rate drops by roughly 7-10% in low‑testosterone states, leaving you with less energy reserve.
The overlap of these mechanisms creates a perfect storm that mimics, and often fuels, chronic fatigue.
Spotting the Hormonal Signature
Because the symptoms are non‑specific, doctors rely on a focused lab panel:
- Total testosterone: < 300 ng/dL suggests deficiency.
- Free testosterone: Adjusted for SHBG levels; more accurate in older men.
- LH & FSH: Both low or inappropriately normal when testosterone is low points to secondary cause.
- Prolactin: Elevated levels can suppress the HPG axis.
Imaging (MRI of the pituitary) is reserved for cases with visual field cuts or abnormal prolactin.
Comparing Symptoms: Secondary Hypogonadism vs Chronic Fatigue
| Feature | Secondary Hypogonadism | Chronic Fatigue Syndrome |
|---|---|---|
| Morning libido | Markedly reduced | Often unchanged |
| Muscle mass loss | Gradual, measurable | Usually absent |
| Sleep quality | Fragmented, early awakenings | Non‑restorative sleep |
| Hormone labs | Low testosterone + low LH/FSH | Normal endocrine panel |
| Post‑exertional malaise | Present but less severe | Core diagnostic criterion |
Managing the Hormone Gap
When labs confirm secondary hypogonadism, treatment aims to restore testosterone while addressing the root pituitary issue.
Testosterone Replacement Therapy (TRT)
- Transdermal gels (5‑10 mg daily) provide steady levels.
- Intramuscular injections (250mg every 2‑3 weeks) are cost‑effective but cause peaks/troughs.
- Monitor hematocrit, PSA, and lipid profile every 3‑6 months.
Pituitary‑Targeted Options
- Gonadotropin‑releasing hormone (GnRH) analogues: Can stimulate LH/FSH release in select cases.
- Cabergoline: Low‑dose dopamine agonist lowers prolactin, indirectly boosting LH.
Lifestyle Levers
Even with medication, habits matter. Aim for:
- Strength training: 3×week lifts increase endogenous testosterone by ~15%.
- Sleep hygiene: Keep the bedroom cool, limit screens after 9pm; aim for 7‑8hours of deep sleep.
- Balanced diet: Include zinc‑rich foods (oysters, pumpkin seeds) and healthy fats (avocado, olive oil).
- Stress reduction: Chronic cortisol suppresses the HPG axis; mindfulness or yoga can help.
When to Seek Professional Help
If you notice any of the following, book an appointment:
- Persistent low energy despite adequate sleep.
- Decreased sexual desire or erectile issues.
- Unexplained loss of muscle tone.
- Laboratory results showing low testosterone with low LH/FSH.
A qualified endocrinologist can run the full hormonal work‑up and tailor therapy.
Bottom Line
Secondary hypogonadism is a silent driver of chronic fatigue for many men. By recognizing the hormonal clues, getting the right labs, and treating the underlying pituitary signal, you can reclaim energy, mood, and quality of life.
Frequently Asked Questions
Can secondary hypogonadism cause fatigue in women?
Yes. Although testosterone levels are lower in women, a pituitary‑driven drop can still affect energy, mood, and muscle strength. Women often present with reduced libido and generalized weakness rather than classic male symptoms.
How long does it take to feel better after starting TRT?
Most men notice improved vigor within 3‑4weeks, but optimal muscle gains and mood stabilization can take 2‑3months. Consistent monitoring ensures doses are right.
Is there a risk of fertility loss with testosterone therapy?
Exogenous testosterone suppresses LH and FSH, which can lower sperm production. Men who wish to preserve fertility should discuss options like gonadotropin therapy or using TRT for a limited period.
What lifestyle changes help the pituitary recover?
Adequate sleep, regular moderate exercise, balanced macronutrients, and stress‑management techniques (meditation, deep‑breathing) can improve endogenous hormone release.
Can chronic fatigue be diagnosed without labs?
Diagnosis relies on clinical criteria (duration, post‑exertional malaise, unrefreshing sleep). However, ruling out medical causes-like secondary hypogonadism-requires targeted lab tests.
Comments (12)
-
Julius Adebowale October 3, 2025
The article oversimplifies hormone mechanics.
-
KISHORE KANKIPATI October 13, 2025
Hey, I get where you’re coming from, but the endocrine system is a kaleidoscope of signals-painting a picture with just a few broad strokes misses the vibrant hues that make each case unique.
-
Ben Wyatt October 23, 2025
If you’re battling that fog, start with the basics: get a full hormone panel (total & free testosterone, LH, FSH, prolactin), prioritize 7‑8 hours of deep sleep, and add a couple of strength‑training sessions a week. Those steps often lift energy levels before you even think about medication.
-
Daniel LaMontagne November 2, 2025
Thanks for the solid steps! 😊 I’ve been tracking my sleep and added a few deadlifts – already feeling a bit more “charged”. Keep the tips coming!
-
Jefferson Vine November 12, 2025
Alright, strap in because we’re about to peel back the layers of the testosterone saga that the mainstream health blogs love to gloss over.
First off, the pituitary isn’t just a passive water cooler; it’s a mastermind that can be subtly hijacked by everything from hidden endocrine disruptors to shadowy pharmaceutical lobbying.
When LH and FSH dip, your testes get the memo to shut down production, and the fallout is a cascade of fatigue that feels like dragging a boulder through molasses.
You might think it’s just a low‑testosterone issue, but the truth is that a suppressed hypothalamic‑pituitary axis can also mute the body’s metabolic fire, slowing mitochondrial engines.
That’s why you wake up feeling like you’ve run a marathon in your dreams, despite actually sleeping eight solid hours.
Add to that the fact that many labs still use outdated reference ranges, allowing borderline cases to slip through the cracks while insurers claim they’re “normal”.
And let’s not ignore the covert pressure from big pharma to push synthetic TRT as the universal fix, while quietly funding research that demonizes the underlying pituitary problem.
Because if you treat the symptom without addressing the signal, you’re just repainting the same old mural with a different color.
I’ve seen patients who, after months on gels, end up with polycythemia and still complain of crushing exhaustion-clear evidence that the root cause was never tackled.
Lifestyle tweaks like high‑intensity interval training, zinc‑rich foods, and stress‑busting meditation can actually recalibrate the HPG axis, something the industry prefers you not to know.
Moreover, emerging peptide therapies that stimulate endogenous hormone release are being sidelined in favor of big‑ticket injections that line corporate pockets.
If you’re skeptical, look at the 2023 Endocrine Society meta‑analysis: men with low LH/FSH but normal testicular size had a 42% higher odds of reporting severe fatigue.
That data point alone should make any rational mind question why the standard of care still hinges on testosterone numbers alone.
In short, think of secondary hypogonadism as a silent saboteur – it’s not just about low testosterone, it’s about a broken communication line.
Fixing it means a thorough work‑up, possibly a pituitary MRI, and a treatment plan that targets the source, not just the symptom.
Stay curious, question the protocols, and remember: the body often whispers its woes long before the labs scream.
-
Christian Miller November 22, 2025
While the exposition is compelling, one must also consider the systematic suppression of alternative therapies by regulatory entities that profit from the prevailing pharmaceutical paradigm, thereby limiting patient access to truly restorative interventions.
-
Donna Oberg December 2, 2025
Wow!!! This whole hypogonadism thing is like a secret underground river of energy that’s been dammed for far too long!!! Your post just pulled back the curtain and let the floodgates roar!!! It’s about time we all wake up and feel the rush!!!
-
Garreth Collard December 12, 2025
One cannot simply skim the surface of endocrine dysregulation without acknowledging the intricate symphony of neuroendocrine feedback loops that orchestrate our very vigor; to reduce this masterpiece to a mere checklist is to do a disservice to both the science and the discerning reader.
-
Gary Levy December 22, 2025
True, the layers are deep, but breaking them down into practical steps-like checking LH/FSH and tweaking sleep hygiene-makes the complexity accessible without diluting its essence.
-
sourabh kumar January 1, 2026
the article misses the point it just repeats typical info no new insight
-
AJIT SHARMA January 11, 2026
Honestly this is just another excuse for men to complain and demand pills while ignoring the real moral duty to push back against a system that profits from our weakness.
-
NORMAND TRUDEL-HACHÉ January 21, 2026
Look, the science is clear – low testosterone means low energy. No need for fancy talk, just get the labs and fix it.
