When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck. It’s the result of strict science-and a regulatory system designed to make sure there’s no difference in how the drug behaves in your body. The U.S. Food and Drug Administration (FDA) doesn’t just accept claims. It demands proof. That proof comes from bioequivalence studies.
What Bioequivalence Really Means
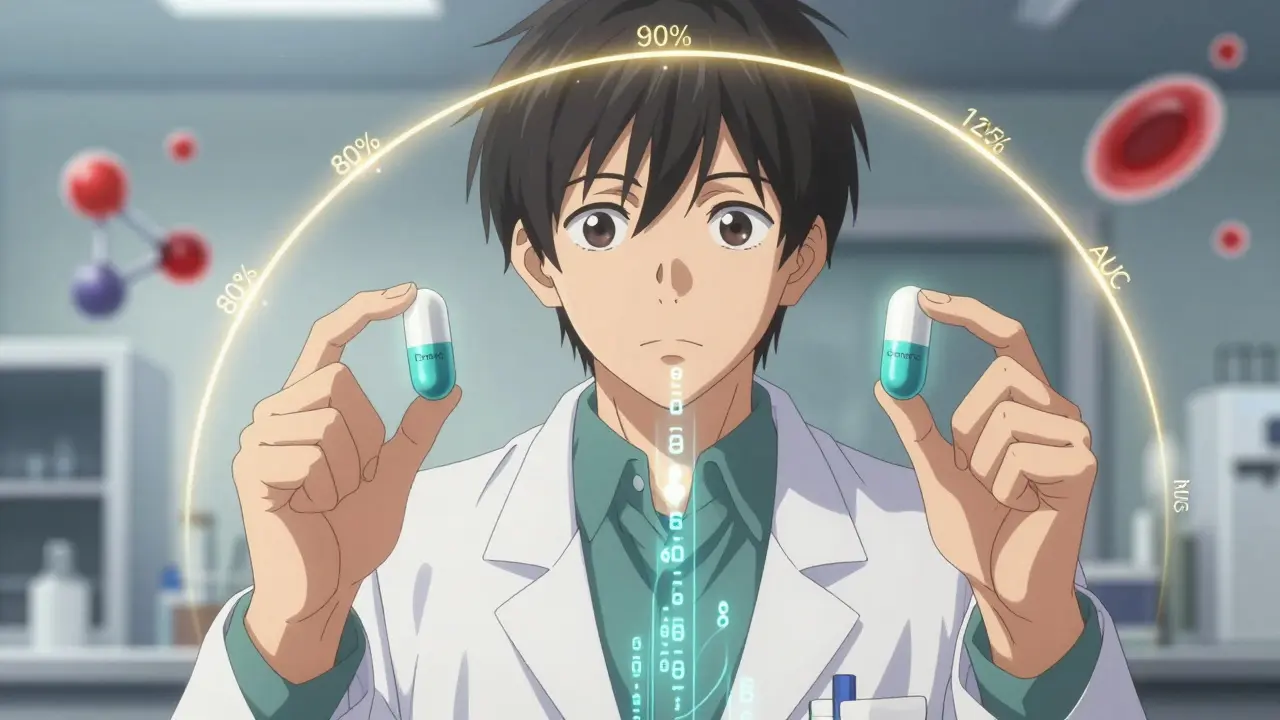
Bioequivalence isn’t about looking the same or having the same ingredients. It’s about whether your body absorbs the drug the same way. Two drugs are bioequivalent if they release the same amount of active ingredient into your bloodstream at the same rate. That means the peak concentration (Cmax) and total exposure over time (AUC) must match closely between the generic and the brand-name version. The FDA’s definition is precise: "The absence of a significant difference in the rate and extent to which the active ingredient becomes available at the site of drug action." In plain terms, if you take a generic drug, your body should react to it just like it would to the original. No more, no less. This isn’t optional. It’s the law. Under the Hatch-Waxman Act of 1984, generic manufacturers don’t have to repeat expensive clinical trials to prove safety and effectiveness. But they must prove bioequivalence. That’s the trade-off: faster, cheaper access to medicines in exchange for solid science.The 80/125 Rule: The Golden Standard
The FDA’s main tool for measuring bioequivalence is the 80/125 rule. It sounds simple, but it’s backed by decades of data and statistical rigor. Here’s how it works: In a clinical study, healthy volunteers take both the generic and the brand-name drug. Blood samples are taken over hours to track how much of the drug enters the bloodstream. The key numbers are Cmax and AUC. The FDA requires that the 90% confidence interval for the ratio of the generic’s values to the brand’s values falls between 80% and 125%. That means if the brand drug delivers 100 units of active ingredient, the generic must deliver between 80 and 125 units. Not 79. Not 126. Between 80 and 125. This range was chosen because it reflects what’s considered clinically insignificant-no meaningful difference in how the drug works in the body. This rule applies to most systemic drugs. But it’s not one-size-fits-all. For drugs with a narrow therapeutic index-like warfarin, levothyroxine, or lithium-the bar is higher. The FDA tightens the range to 90-111%. Why? Because even small changes in blood levels can cause serious side effects or make the drug ineffective. There’s no room for error.How the Studies Are Done
Most bioequivalence studies involve 24 to 36 healthy adults. They’re given the generic and brand-name versions in a crossover design-meaning each person takes both, but in a random order, with a washout period in between. This reduces individual variability. The study is usually done under fasting conditions. Why? Because food can change how a drug is absorbed. If the brand-name drug is meant to be taken with food, the generic must also be tested under fed conditions. The FDA requires both scenarios when necessary. The lab work is just as important as the human part. Blood samples are analyzed using validated, highly sensitive methods-often mass spectrometry. The FDA requires full documentation of every step: how samples were stored, how the lab calibrated equipment, how data was processed. A single mistake in handling can invalidate the whole study. And it’s expensive. A single bioequivalence study can cost between $500,000 and $2 million. That’s why many manufacturers look for ways to cut corners-only to get rejected by the FDA.
When You Don’t Need a Human Study: Biowaivers
Not every drug needs a full clinical trial. The FDA allows biowaivers for certain products where absorption is predictable and unlikely to vary. For example:- Oral solutions with the same active and inactive ingredients as an approved product
- Topical products meant to work locally on the skin, not absorbed into the blood
- Inhalant anesthetics that are volatile gases
- Q1: Same active and inactive ingredients
- Q2: Same dosage form and strength
- Q3: Same pH, solubility, and dissolution profile
Why So Many Applications Get Rejected
Despite the clear rules, the FDA’s first-cycle approval rate for generic drug applications (ANDAs) was just 43% in 2022. That means nearly 6 out of 10 submissions failed on the first try. Common reasons?- Wrong study design-too few participants, no fasting/fed arms when needed
- Poor analytical methods-lab tests that aren’t sensitive or accurate enough
- Missing documentation-no clear chain of custody for blood samples
- Ignoring product-specific guidances (PSGs)

What’s Changing in 2026
The FDA is updating its approach for complex drugs-things like inhalers, topical creams, and drug-device combos. These aren’t simple pills. Their absorption depends on how they’re applied, how they dissolve, or how they’re delivered. New tools are being used:- Physiologically Based Pharmacokinetic (PBPK) modeling-computer simulations that predict how a drug behaves in the body without human trials
- In vitro permeation testing (IVPT)-measuring how a cream penetrates skin layers in the lab
- Scaled Average Bioequivalence (SABE)-a flexible method for highly variable drugs where the 80/125 rule doesn’t fit
Why This Matters to You
Generic drugs make up 90% of prescriptions in the U.S. but cost only 23% of what brand-name drugs do. That’s billions saved every year. But that savings only works if the generics are truly equivalent. Bioequivalence studies are the invisible guardrail. They’re why you can switch from brand to generic without worrying about your blood pressure spiking, your seizures returning, or your thyroid levels going haywire. The FDA doesn’t just approve drugs. It validates trust. And that trust is built on data, not promises.Do generic drugs work as well as brand-name drugs?
Yes-if they’ve passed FDA bioequivalence testing. The FDA requires that generics deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name drug. Studies show no meaningful difference in effectiveness or safety when bioequivalence criteria are met. Over 90% of U.S. prescriptions are filled with generics because they’re proven to work the same way.
What happens if a generic drug fails bioequivalence testing?
The FDA issues a Complete Response Letter, outlining exactly what’s missing or flawed. The manufacturer must fix the issue-whether it’s redesigning the formulation, running a new study, or improving lab methods-and resubmit. Many companies go through multiple rounds before approval. There’s no shortcut.
Are all generic drugs tested on humans?
No. For certain products like topical creams, eye drops, or oral solutions with identical ingredients, the FDA allows biowaivers. These rely on in vitro tests and chemical comparisons instead of human trials. But for most oral pills and injectables, human studies are required.
Why does the FDA use 80-125% instead of 100%?
No two formulations are exactly identical in how they dissolve or absorb. The 80-125% range accounts for normal biological variation and minor manufacturing differences. It’s based on decades of clinical data showing that within this range, therapeutic outcomes are equivalent. Going outside it would mean a real risk of under- or overdosing.
Can a generic drug be approved without any clinical data?
Yes, but only for very specific cases. Biowaivers apply to products like parenteral solutions, ophthalmic drops, or topical creams with no systemic absorption. These rely on matching chemical properties and dissolution profiles. For drugs meant to enter the bloodstream, clinical data from human studies is mandatory.
Comments (14)
-
Alexandra Enns January 25, 2026
Let me stop you right there-this whole bioequivalence thing is a scam. I’ve seen generics make my cousin’s seizures worse. The FDA doesn’t care about real people, they care about corporate profits. 80-125%? That’s a license to poison people with cheaper junk. I’ve got a PhD in pharmacology and I’m telling you-this isn’t science, it’s capitalism with a lab coat.
-
Marie-Pier D. January 27, 2026
Wow, this is actually so important and so well explained 💙 I’ve been on generics for 12 years and never knew how much science went into making sure they’re safe. Thank you for breaking this down-it’s easy to be skeptical, but this makes me trust the system again. Keep sharing gems like this!
-
Patrick Gornik January 27, 2026
Ah yes, the sacred 80/125 rule-the Hegelian dialectic of pharmaceutical regulation. The thesis being brand-name monopolies, the antithesis being generic commodification, and the synthesis? A regulatory fiction masquerading as scientific rigor. The FDA doesn’t validate trust-it manufactures consent through statistical sleight of hand. And don’t get me started on PBPK modeling: it’s not predictive science, it’s algorithmic mysticism dressed in pharmacokinetic garb.
-
Sawyer Vitela January 29, 2026
First-cycle approval rate 43%. That’s not a bug, it’s a feature. Waste $2M, get rejected, try again. Profit.
-
Izzy Hadala January 29, 2026
Could you please clarify whether the 90% confidence interval for Cmax and AUC is calculated using log-transformed data? The FDA’s guidance documents specify this, but it’s often omitted in public summaries. Also, is the sample size of 24–36 subjects sufficient for highly variable drugs under SABE? I’m curious about the statistical power assumptions.
-
Elizabeth Cannon January 30, 2026
ok so i read this whole thing and i’m not mad anymore. i used to think generics were just ripoffs but now i get it-this is wild how much work goes into it. i work in retail and people complain about generic pills all the time, now i got facts to throw back at em 😎
-
Gina Beard January 31, 2026
It’s not about trust. It’s about control.
-
Don Foster February 1, 2026
Biowaivers are just lazy science. If it’s not tested on humans it’s not real. The FDA is letting pharma cut corners and calling it innovation. And don’t even get me started on Q1-Q2-Q3-sounds like a bad IKEA manual
-
siva lingam February 3, 2026
so you paid 2 million dollars to prove that a pill is a pill? wow. what a country. i could’ve told you that for free
-
Shelby Marcel February 5, 2026
wait so if i take a generic for my anxiety and it feels different… is that just in my head? or did the lab mess up the dissolution profile? i’ve been wondering this for years
-
blackbelt security February 7, 2026
People underestimate how hard this is. Every drop of blood, every calibration, every hour of fasting-this is the invisible work that keeps you alive. Respect the process.
-
Tommy Sandri February 8, 2026
While the regulatory framework is robust, one must acknowledge the cultural implications of generic drug adoption in low-income populations. Access is not merely a technical issue-it is a socioeconomic imperative. The FDA’s role transcends pharmacokinetics and enters the domain of public equity.
-
Karen Conlin February 9, 2026
Thank you for writing this. I’m a nurse and I’ve seen patients panic because their generic pill looks different-even though it’s the same chemistry. This post should be printed and handed out in every pharmacy. Also-can we please stop calling the 80-125 rule ‘lenient’? It’s not. It’s the result of decades of real-world data showing that outside that range, you risk toxicity or therapeutic failure. The people who say ‘it should be 100%’ have never seen someone overdose on warfarin because their INR spiked. This isn’t theory. It’s life or death.
And to the guy who said ‘it’s just a pill’-you’re right. But it’s also the only thing standing between someone and a hospital bed. Don’t dismiss it.
-
Sushrita Chakraborty February 9, 2026
While the FDA’s bioequivalence standards are indeed rigorous, one must also consider the global disparity in regulatory frameworks. In many low- and middle-income countries, bioequivalence testing is either absent or performed with substandard methodologies. The 80–125% range, while scientifically sound in controlled environments, may not be adequately translatable to populations with significant metabolic variability due to diet, genetics, or comorbidities. Therefore, while the U.S. model is exemplary, it cannot be universally applied without contextual adaptation.
