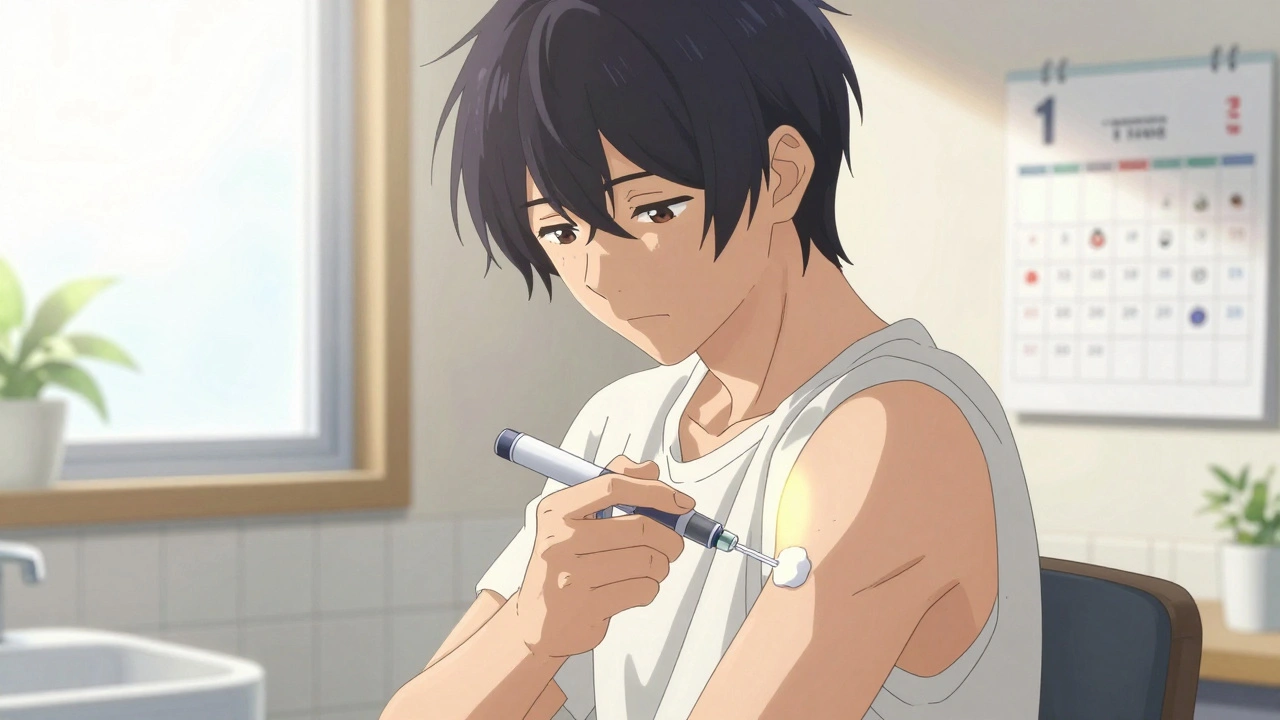
When you’re prescribed a biologic therapy, you’re not just getting a powerful drug-you’re being handed responsibility for your own treatment. These medications, made from living cells, are used for conditions like rheumatoid arthritis, psoriasis, Crohn’s disease, and multiple sclerosis. They’re effective, but they come with a catch: you have to inject them yourself. And if you don’t do it right, you risk more than just a bad day-you risk infection, treatment failure, or even hospitalization.
Why Injection Training Isn’t Just a Formality
Most patients think training is a quick demo: the nurse shows you how to press the button, you mimic it once, and you’re sent home with a box of pens. But that’s not training. That’s a gamble. According to a 2022 study, 91.7% of patients say they got some kind of instruction-but only 27% received full training that included telling (explanation), showing (demonstration), and doing (hands-on practice). The rest? They’re flying blind. The stakes are high. One in three patients report feeling unsure about their technique within the first six months. And when you’re unsure, you hesitate. You skip doses. You rush. You inject in the wrong spot. That’s how infections start.How Infections Happen-And How to Stop Them
Infection isn’t just about dirty hands. It’s about broken sterile technique. The CDC says improper injection technique increases the risk of skin and soft tissue infections by 37%. That means redness, swelling, warmth, pus, or fever aren’t just inconvenient-they’re warning signs. Here’s how it goes wrong:- You skip wiping the skin with alcohol-or you wipe it, then touch it before injecting.
- You reuse a needle (even once) because you’re afraid to use a new one.
- You inject over a bruise, scar, or rash, thinking it’s fine.
- You don’t rotate injection sites, so the same spot gets poked every week.
- You don’t check the solution before injecting-cloudy or discolored biologics can mean contamination.
- Wash your hands with soap for 20 seconds. No hand sanitizer. Soap removes more germs.
- Use a fresh alcohol swab each time. Let the skin dry completely-don’t blow on it.
- Choose clean, healthy skin: abdomen (2 inches from the navel), thighs, or upper arms. Never inject over veins, scars, or tattoos.
- Rotate sites. Keep at least one inch between each injection. Write down where you injected last time.
- If the liquid looks cloudy, has particles, or is discolored-don’t use it. Call your pharmacy.
What Real Training Looks Like (And Why Most of It Fails)
Good training isn’t a 30-minute rush. It’s a process. The best programs follow the TEACH model:- Tell: Explain why each step matters. Not just “press here,” but “this releases the needle safely.”
- Enable: Give you a training device-same size, same weight, same click-as the real one. No medication. Unlimited practice.
- Act: Let you do it. Watch. Correct. Don’t just nod. Say, “Show me how you’d do this at home.”
- Check: Use the teach-back method. Ask you to explain the steps in your own words. If you can’t, you didn’t learn it.
- Help: Connect you to follow-up support-phone, video call, or in-person check-ins.

The Hidden Problem: Anxiety Is Your Biggest Enemy
It’s not the needle. It’s the fear. People don’t stop injecting because they can’t do it. They stop because they’re scared. A 2021 study found that emotional stress causes 57% of early treatment drops. You’re not weak for feeling this. It’s normal. But you need tools. Try this: Build a ritual. Same time. Same place. Same sequence. Light a candle. Play your favorite song. Breathe in for four counts, hold for four, out for six. Do it before every injection. It’s not superstition-it’s neuroscience. Rituals calm your nervous system. Also, ask for the “breathing room” technique: Have someone gently rest their hand over yours as you inject. It stops you from jerking the device too early. It works for 88% of anxious patients.What You Should Ask Your Provider
Don’t wait until you’re confused. Ask these questions before your first injection:- “Can I practice with a trainer device until I feel confident?”
- “Will I get a video or app I can watch again?”
- “Who do I call if I’m not sure I did it right?”
- “Can I schedule a follow-up visit in two weeks to show you how I’m doing?”
- “What signs of infection should I watch for?”

What’s Changing-And What’s Working Now
The industry is waking up. In 2023, the FDA released new draft guidelines pushing for standardized training. Some drugmakers are rolling out digital platforms with video tutorials, virtual coaching, and injection trackers. Adbry, for example, now offers a free app with step-by-step videos and reminders. But the biggest breakthrough? Teaching rituals. Patients who built a consistent routine had 53% fewer technique errors and 41% better adherence over six months. That’s not magic. That’s structure.What to Do Right Now
If you’re starting biologic therapy:- Request a full training session-no shortcuts.
- Ask for a training device. Practice until you can do it blindfolded.
- Write down your injection routine: time, place, steps.
- Keep a log of each injection site. Use a calendar or app.
- Set a reminder for a follow-up check-in two weeks after your first injection.
- Know the signs of infection: redness over 2 cm, warmth, swelling, fever above 100.4°F.
Final Thought: You’re Not Alone
Thousands of people inject biologics every day. Most of them were terrified at first. Most of them got better-not because they were brave, but because they learned the right way. You can too. This isn’t about being perfect. It’s about being prepared. One wrong move can cost you weeks of treatment. But one good habit-like washing your hands, rotating sites, or asking for help-can keep you on track for years.Can I reuse a biologic injection needle if I only used it once?
No. Biologic needles are single-use only. Reusing even once can dull the tip, increase pain, and introduce bacteria into your skin. Always use a new, sterile needle for every injection. Never recycle or store used needles for later use.
What should I do if I see redness after injecting?
If the redness is smaller than 2 cm and fades within a day, it’s likely minor irritation. But if it’s larger, warm to the touch, swollen, or getting worse after 24 hours, call your doctor. These could be early signs of infection. Don’t wait. Early treatment prevents serious complications.
Is it safe to inject if I’m sick or have a fever?
Generally, no. If you have a fever over 100.4°F, an active infection, or are on antibiotics, delay your injection. Biologics suppress your immune system. Injecting while sick can make your infection worse or mask symptoms. Call your provider before injecting if you’re unwell.
Can I inject in the same spot if I rotated last week?
No. Even if you rotated last week, you should still avoid reusing the exact same spot too soon. Wait at least 1 inch from your last injection site, and ideally, wait a full week before returning to the same general area. Repeated injections in the same spot can cause tissue damage, lumps, or poor drug absorption.
What if I accidentally inject into a vein?
Biologic injections are meant for subcutaneous tissue, not veins. If you see blood in the syringe or pen after inserting the needle, stop immediately. Do not inject. Remove the device and dispose of it safely. Use a new pen or syringe and choose a different site. If you’re unsure, call your healthcare provider. Injecting into a vein can cause serious side effects, including rapid immune reactions.
Are there apps or tools that help track injections?
Yes. Many biologic manufacturers offer free apps with injection reminders, site maps, and symptom trackers. For example, Adbry and Enbrel have digital tools that let you log each injection, see your rotation pattern, and get video tutorials. You can also use any calendar app-just label each day with the site you used. Tracking helps you avoid mistakes and gives your doctor useful data.
How do I know if my training was good enough?
If you were able to practice with a trainer device, explain each step in your own words, received feedback, and had access to follow-up support, your training was likely sufficient. If you were only shown once, given no practice tool, and told to “figure it out,” it wasn’t. Good training leaves you feeling confident, not confused. Don’t hesitate to ask for more help.
Comments (13)
-
Michaux Hyatt December 11, 2025
Just wanted to say this post saved my life. I was skipping doses because I was terrified of messing up-then I found the TEACH model and started practicing with a trainer pen every morning before coffee. Now I’m six months in, zero infections, and I even taught my mom how to help me rotate sites. You’re not alone out there.
-
Raj Rsvpraj December 11, 2025
Pathetic. In India, we’ve been injecting biologics for decades without ‘training sessions’-we use our hands, we use our minds, we use our discipline. You Americans need a 20-minute video and a branded app to press a button? How did we survive before Big Pharma invented ‘anxiety’ as a medical condition?
-
Jack Appleby December 12, 2025
Let’s be precise: the 91.7% statistic is misleading because it conflates ‘instruction’ with ‘competency assessment.’ The CDC’s 37% increased infection risk is derived from a meta-analysis of six studies with heterogeneous sampling-most from tertiary centers, not community clinics. And let’s not forget: the ‘TEACH’ model was developed by a team at Johns Hopkins with NIH funding; it’s not some corporate buzzword. Also, ‘blow on it’? That’s not just unhygienic-it’s microbiologically indefensible. The evaporation rate of alcohol on skin is 0.8 seconds per mL under ambient conditions; blowing disrupts laminar flow and reintroduces oropharyngeal flora. Do better.
-
Frank Nouwens December 13, 2025
Thank you for this comprehensive and deeply thoughtful guide. I’ve been administering biologics for over three years, and I wish I’d had this resource when I started. The emphasis on ritual and emotional regulation resonates profoundly. I’ve begun lighting a candle before each injection-it’s become a quiet, grounding moment in an otherwise chaotic day. Small things, indeed, make all the difference.
-
Kaitlynn nail December 14, 2025
It’s not about the needle. It’s about the fear. And fear? It’s just love that forgot how to breathe.
-
Aileen Ferris December 14, 2025
wait so you’re telling me i’m not supposed to reuse needles? but my cousin’s aunt’s neighbor did it for 3 months and still got a tattoo on her thigh so… idk?? maybe the docs are just trying to sell more pens??
-
Michelle Edwards December 15, 2025
I know how scary this feels. I remember my first injection-I cried. But I kept a little journal: ‘Day 1: abdomen, felt shaky. Day 2: thigh, did the breathing thing. Day 3: arm, didn’t touch the swab after.’ You’re not failing. You’re learning. And every time you show up? That’s courage.
-
David Palmer December 17, 2025
why is everyone so dramatic about this? i just poke myself and move on. if i get an infection, i get an infection. life’s not a safety video. also, who cares if the liquid looks cloudy? i shake it and it’s fine.
-
Vivian Amadi December 19, 2025
So you’re telling me I’m supposed to write down where I injected? And use a calendar? And CALL MY DOCTOR? Are you serious? This is why people hate healthcare. You turn a simple needle into a full-time job. I’m not a nurse. I’m not a robot. I’m a person with a life.
-
Jimmy Kärnfeldt December 20, 2025
There’s something beautiful in how something so clinical-like a shot-can become sacred when you give it space. The ritual isn’t about control. It’s about tenderness. You’re not just injecting medicine. You’re saying, ‘I’m still here. I’m still fighting.’ And that matters more than any protocol.
-
Ariel Nichole December 22, 2025
Love this. I’ve been using the Adbry app and it’s honestly a game-changer. I get nudges to rotate sites and even little emojis when I log a successful injection. Feels like a mini victory. Also, the video tutorials? So much clearer than the nurse’s 5-minute demo. Thanks for sharing this!
-
Neelam Kumari December 22, 2025
Oh, so now we need apps and candles and breathing exercises to inject a drug? How quaint. My grandmother injected insulin in 1972 with a syringe she boiled in water and a pocket watch. You people are weak. And this ‘TEACH’ nonsense? It’s just corporate branding dressed up as care.
-
Queenie Chan December 23, 2025
Okay, but what if your skin is so scarred from years of injections that there’s literally no ‘clean’ spot left? I’ve been on this for 8 years. My abdomen looks like a topographical map of failed attempts. Do I just… stop? Or do I start injecting into my buttocks like a cowboy with a syringe? Because I’m out of options and my doctor keeps saying ‘rotate more.’ But there’s no ‘more.’
