When a pharmacist hands over a prescription for a controlled substance, they’re not just filling a order-they’re stopping a potential overdose, a diversion, or even a death. The stakes are real. Every year, thousands of prescriptions are filled with errors in quantity or directions, and those mistakes don’t just vanish. They end up in the wrong hands, in the wrong doses, with deadly consequences. The DEA reports that improper verification contributed to over 6,200 enforcement actions between 2018 and 2023. That’s not a statistic-it’s a pattern of preventable harm.
What Exactly Must Be Verified?
You can’t verify what you don’t know to look for. Federal law under 21 CFR § 1306.05 requires seven specific elements on every controlled substance prescription. Missing even one can mean the difference between compliance and legal liability. These are non-negotiable:- Prescriber’s full name and address - No abbreviations. No initials. If it’s not spelled out, ask.
- Date of issuance - Schedule II prescriptions must be dated the day they’re presented. For Schedules III-V, the date can’t be more than six months old.
- Patient’s full name and address - Middle names matter. Address changes? Verify it matches the pharmacy’s records.
- Drug name and strength - Is it oxycodone 5 mg or 10 mg? A single digit can mean the difference between pain relief and respiratory arrest.
- Dosage form - Tablet, capsule, liquid, patch? The form changes how the drug is absorbed.
- Quantity prescribed - This is where most errors happen. The number must match the written word. If it says "thirty (30) tablets," both must agree. CMS data shows 2% of Medicaid rejections in 2022 were due to mismatched quantities.
- Directions for use (sig) - "Take one by mouth every 6 hours as needed for pain" isn’t vague. "Take 1 q6h PRN" is acceptable. But "take as needed" without frequency? That’s a red flag.
These aren’t suggestions. They’re the legal minimum. Skip one, and you’re opening yourself-and your pharmacy-to civil penalties up to $758,574 per violation, or worse, criminal charges.
DEA Number Validation: The Three-Step Check
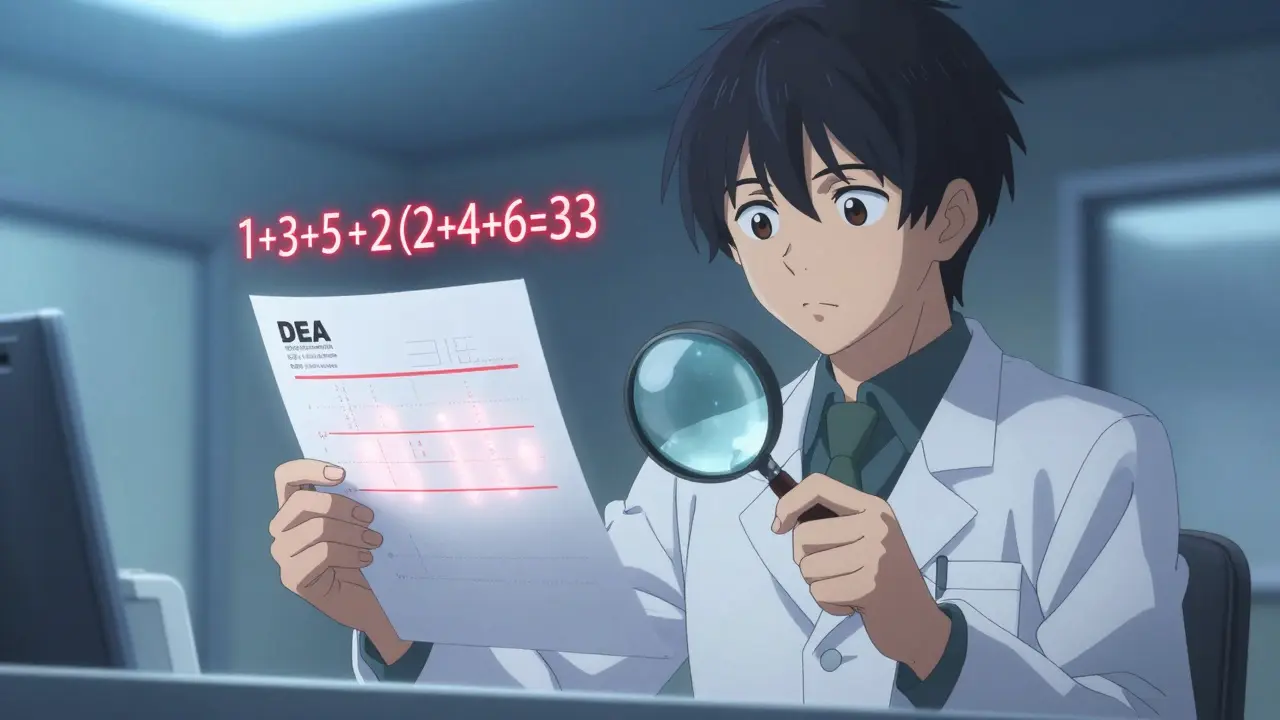
A DEA number looks like this: AB1234567. But not every number ending in 7 is valid. The DEA built a math-based system to catch forgeries. Here’s how to verify it in under 30 seconds:- Check the second letter - It must match the prescriber’s last name initial. If the prescriber is Dr. Smith, the second character must be an S. If it’s a J, stop. Ask for proof.
- Add the 1st, 3rd, and 5th digits - In AB1234567, that’s 1 + 3 + 5 = 9.
- Add the 2nd, 4th, and 6th digits, then double the sum - 2 + 4 + 6 = 12. Multiply by 2 = 24.
- Add the two results - 9 + 24 = 33. The last digit (3) must match the 7th digit of the DEA number. In this case, it does: 3.
This method catches 98.7% of fake DEA numbers, according to DEA validation studies. If the math doesn’t add up, don’t guess. Call the prescriber. Use the DEA’s free OSCAR system to look up valid registrants. And never, ever accept a DEA number without the prescriber’s name matching.
Quantity and Directions: The Hidden Trap
A prescription might say "120 tablets" and "take 2 every 8 hours." Sounds fine. But if the patient is on methadone, and this is a refill, you’ve got a problem. Methadone conversion factors vary by daily dose: 4 for under 20 mg/day, 8 for 21-40 mg/day, 10 for 41-60 mg/day, and 12 for over 61 mg/day. If the patient was previously on 40 mg/day and now has a 120-tablet prescription of 10 mg tablets, that’s 1,200 mg total. That’s 120 mg/day. That’s 3x their previous dose. That’s not a refill-it’s a risk.That’s why CDC opioid conversion factors aren’t optional. They’re part of clinical verification. Same with fentanyl patches. A 25 mcg/hr patch equals 60 mg oral morphine per day. If the patient is also getting oral oxycodone 30 mg three times daily (90 mg/day), you’re looking at a total daily morphine equivalent of 150 mg. That’s above the CDC’s recommended threshold for high-risk prescribing. You need to flag this.
Handwritten prescriptions? They’re the #1 source of errors. A 2023 Pharmacy Times survey found 68% of pharmacists struggle with illegible handwriting. One pharmacist in Sydney told me she once filled a prescription that read "50 mg"-but the doctor meant "5 mg." The patient nearly died. Now she uses a 10x magnifier on every handwritten script. Microprinting, asterisk borders, and check-off boxes are security features. If the paper doesn’t have them, it’s not compliant.

PDMP: The Real-Time Lifeline (and Its Flaws)
Prescription Drug Monitoring Programs (PDMPs) are supposed to be your first line of defense. In 49 states, you’re legally required to check them before dispensing. But here’s the catch: not all PDMPs are equal.Only 27 states require real-time data submission-meaning the prescription shows up in under 5 minutes. The other 22? Some take 24 hours. A few still allow weekly updates. That’s not just slow-it’s dangerous. The DEA’s 2022 diversion report found that 1,247 cases of inappropriate prescribing were directly tied to delayed PDMP data. A patient could get a script from three different doctors in one day, and your system wouldn’t know until tomorrow.
That’s why you can’t rely on PDMP alone. Use it as one of three verification touchpoints. Combine it with DEA number validation and direct prescriber contact. NABP’s PMP InterConnect platform is the gold standard-used by 92% of chain pharmacies and rated 4.7/5 by pharmacists. It cuts verification time by 37%. But if your state’s PDMP lags behind, you’re still responsible. The law doesn’t care if the data is late.
The 5-Point Verification Protocol
The American Society of Health-System Pharmacists (ASHP) and former DEA Director Dr. John R. Overstreet agree: one check isn’t enough. You need a system. Here’s the 5-point protocol used by compliant pharmacies:- Validate the DEA number - Use the math method. Confirm the letter matches the prescriber’s last name.
- Review the PDMP - Look for recent prescriptions from other providers. Check for overlapping opioids, benzodiazepines, or high daily morphine equivalents.
- Assess physical integrity - Is the prescription on security paper? Are there tamper-evident features? Are quantities written in both numbers and words?
- Contact the prescriber - If anything looks off-quantity too high, directions unclear, patient not in records-call. Don’t assume. Don’t guess. Just call.
- Evaluate clinical appropriateness - Use CDC conversion factors. Does this dose make sense for this patient’s history? Are they on multiple high-risk medications? If you’re unsure, consult the prescriber or a clinical pharmacist.
This isn’t extra work. It’s your legal shield. The FDA found that pharmacies using this full protocol had 4% diversion incidents. Those that skipped even one step? 31%.

What’s Changing in 2024 and Beyond
The rules are tightening. By November 27, 2023, all pharmacies must comply with the DSCSA, which requires electronic verification of product identifiers on every package. That means scanning barcodes to confirm the drug isn’t counterfeit. And by 2026, the DEA is rolling out QR codes on all controlled substance prescriptions. These codes will link to the prescriber, the date, the quantity, and the patient-verified in real time.Meanwhile, AI is being tested. Pilot programs in 12 states are using machine learning to flag patterns: a patient getting 10 different opioid scripts from 6 prescribers in 30 days? The system auto-alerts. But the AMA is pushing back, citing privacy concerns. For now, you still need human judgment.
And yes, the costs are rising. The Congressional Budget Office estimates each pharmacy will pay $4,200 more per year by 2030. But they also project those costs will prevent $12.7 billion in healthcare expenses from overdoses and addiction. That’s not just compliance-it’s lifesaving.
Final Checklist: Before You Dispense
Use this every time. Print it. Tape it to your counter.- ✅ Prescriber name and address match DEA registration
- ✅ DEA number math checks out (second letter + digit sums)
- ✅ Patient name and address match pharmacy records
- ✅ Quantity: numbers and words match
- ✅ Directions are clear and clinically appropriate
- ✅ PDMP reviewed (even if data is delayed)
- ✅ CDC conversion factors applied (especially for opioids)
- ✅ Prescription has security features (microprinting, check boxes, asterisks)
- ✅ Prescriber contacted if anything is unclear
- ✅ Dispensed quantity matches prescription (no rounding up)
If you can’t answer "yes" to all 10, don’t dispense. Call. Verify. Wait. It’s better to delay a refill than to risk a life.
What happens if I dispense a controlled substance without verifying the quantity?
You could face license suspension, civil penalties up to $758,574 per violation, or criminal prosecution. The DEA treats quantity mismatches as potential diversion. In 2022, 38% of pharmacy inspections found verification deficiencies, and 52% of independent pharmacies failed compliance. Even one error can trigger an audit or investigation.
Can I rely solely on my pharmacy software to verify prescriptions?
No. While electronic systems catch 99.2% of errors, they can’t replace human judgment. Software may miss illegible handwriting, mismatched DEA letters, or clinical red flags like opioid stacking. The DEA requires pharmacists to personally verify-not just approve a digital alert. Your license is on the line.
Do I need to check the PDMP for every controlled substance, even if it’s a refill?
Yes. State law requires PDMP checks for all Schedule II-V prescriptions, regardless of refill status. A refill doesn’t mean it’s safe. A patient could have received another script from a different doctor since their last fill. In 18 states, PDMP data can be up to 24 hours old-so you’re still working with outdated information. Always check.
What should I do if the prescriber’s DEA number doesn’t match their name?
Do not dispense. Call the prescriber’s office directly to confirm the DEA number. If they can’t provide a valid one, refuse the prescription. DEA numbers are tied to individual practitioners. A mismatch could mean a forged script, a stolen number, or a fraud ring. The DEA’s 2021 study showed 98.7% of invalid DEA numbers are caught with the three-step math check-so if the math fails, it’s not a glitch. It’s a red flag.
Is it okay to round up a quantity if the prescription says "28 tablets" but I only have 30 in stock?
No. You must dispense the exact quantity prescribed. Rounding up-even by two tablets-is a violation. The DEA requires exact matching of written and numerical quantities. If you don’t have 28, call the prescriber for a new script or wait for stock. Dispensing extra is considered diversion under federal law, even if well-intentioned.
Comments (10)
-
Random Guy February 7, 2026so like... i just filled a script for oxycodone and the prescriber wrote "20 (twenty)" but the DEA number was AB1234567 and the second letter was a J?? i double checked the name and it was Dr. JONES. i almost cried. this post is my new bible. thanks for existing.
-
Brett Pouser February 9, 2026man, i’ve been a pharmacist for 12 years and i still get nervous every time a handwritten script comes in. one time i thought "q6h" meant every 6 days. turned out it was 6 hours. patient was fine, but i almost quit. we all mess up. the key is not to be perfect-just vigilant. and yeah, call the prescriber. they’d rather you call than bury someone.
-
Andy Cortez February 10, 2026ok but like... who even uses the math method anymore? i’ve got an app that scans the barcode and auto-verifies the DEA number. why are we still doing addition like it’s 2003? also-PDMPs are a joke. my state updates once a week. i had a guy get 3 scripts in one day and i didn’t know until the next friday. the system is broken.
-
Joseph Charles Colin February 11, 2026From a clinical pharmacy standpoint, the CDC morphine equivalent dose (MED) thresholds are non-negotiable. A total daily MED >90 mg is a red flag per CDC Guideline 2022. When you see concurrent benzodiazepine co-prescribing with opioids, the risk multiplier is 3.7x. Also, fentanyl patch conversions require calculation by body weight-12.5 mcg/hr is not equivalent to 50 mg oral morphine. It’s 37.5 mg. Many EHRs auto-populate this wrong. Always validate manually. Your liability is not worth the shortcut.
-
Tori Thenazi February 12, 2026I’ve been saying this for years. THE DEA IS USING THIS TO TRACK US. EVERY TIME YOU CALL A PRESCRIBER, THEY’RE LOGGING IT. EVERY PDMP CHECK? THAT’S A DIGITAL FINGERPRINT. THEY’RE BUILDING A DATABASE OF EVERY PHARMACIST WHO "DID THEIR JOB"-AND THEN THEY’LL USE IT TO TARGET US FOR "EXCESSIVE VERIFICATION." THEY SAY IT’S FOR SAFETY... BUT WHAT IF THEY JUST WANT TO CONTROL THE FLOW OF MEDS? THEY DID IT WITH CANNABIS. THEY’LL DO IT WITH OXY. I’M NOT RISKING MY LICENSE FOR A GOVERNMENT TRAP.
-
Marie Fontaine February 12, 2026this is so helpful!! 😊 i just started as a tech and was terrified of controlled substances. now i print out the 5-point checklist and stick it on my station. also-i use a 10x magnifier too! 🙌 i once thought "50 mg" was "5 mg"... turned out it was 50. patient was fine. but i cried. thanks for saving me from myself 💖
-
Ken Cooper February 14, 2026i love that you mentioned microprinting. i had a script once where the "100" was printed with a tiny border-i didn’t notice until i held it under a UV light. turned out it was fake. the prescriber’s real number was AB1234567, but the script had AB1234568. i called the office. they said "oh yeah, that’s our intern’s handwriting." i almost fired him. point is: if it looks off, it probably is. always double check. no shame in being extra.
-
Susan Kwan February 15, 2026you say "call the prescriber" like it’s easy. try calling a rural clinic at 4:45 PM on a Friday when they’ve already closed and you’re the last one in the pharmacy. no one answers. you’ve got a patient in front of you, 70 years old, in pain, and your manager is breathing down your neck. so you dispense. because you’re not a robot. and the system doesn’t care about your humanity. this checklist is great... but it’s not real life.
-
Randy Harkins February 16, 2026this is exactly the kind of content we need more of. 🙏 thank you for laying it out so clearly. i’ve been in this field for 15 years and i still learn something new every week. the 5-point protocol? i’ve started using it with my team. we even do a 5-minute daily huddle to review one red flag. it’s changed our error rate by 60%. you’re not just helping pharmacists-you’re saving lives. seriously, thank you.
-
Chima Ifeanyi February 17, 2026Let’s be real. This entire regulatory framework is a performance metric for bureaucrats. The DEA doesn’t care if you save a life-they care if your logs are compliant. The 2% Medicaid rejection rate? That’s not a failure of verification-it’s a failure of incentivization. Why should a pharmacist risk their career when the reimbursement for verification is $0.03 per script? The system is designed to punish diligence, not reward it. The real solution? Decriminalize all controlled substances. Then we can stop pretending this is about safety and admit it’s about control.
