
Multiple sclerosis isn’t just a neurological condition-it’s an internal betrayal. Your own immune system, designed to protect you, turns against your brain, spinal cord, and optic nerves. It doesn’t fight off viruses or bacteria. Instead, it targets the protective coating around your nerve fibers-myelin-and slowly dismantles the wiring that lets your body move, feel, and think. This isn’t random damage. It’s a targeted, chronic autoimmune attack.
What Happens When the Immune System Goes Rogue
In a healthy body, immune cells patrol for threats and leave the central nervous system alone. The blood-brain barrier acts like a security checkpoint, letting in only what’s necessary. But in multiple sclerosis, that barrier gets breached. Immune cells-mainly T cells and B cells-slip through and start attacking myelin, the fatty insulation that wraps around nerve fibers like plastic on an electrical wire. Without myelin, nerve signals slow down or stop entirely. That’s when symptoms show up: blurred vision, numbness in limbs, trouble walking, or sudden fatigue. The immune system doesn’t just attack once. It keeps coming back. Each flare-up leaves behind scar tissue-sclerosis-which is where the disease gets its name. Over time, these scars add up. Nerves lose their ability to communicate, and damage becomes permanent. Research shows this isn’t just one type of attack. There are at least four different patterns of damage seen in MS patients. In some, T cells dominate. In others, antibodies from B cells play a bigger role. One pattern even shows oligodendrocytes-the cells that make myelin-dying off without clear signs of immune invasion. This complexity is why treatments don’t work the same for everyone.Who Gets MS and Why
About 2.8 million people worldwide live with MS. Women are two to three times more likely to be diagnosed than men. It’s not just gender-location matters too. In Scandinavia and Canada, rates jump to 140 cases per 100,000 people. In parts of Asia and Africa, it’s under 5 per 100,000. That gap points to environmental triggers working with genetic risk. The biggest environmental clue? Epstein-Barr virus. People who’ve had this common virus-mononucleosis-are 32 times more likely to develop MS. That doesn’t mean EBV causes MS, but it’s a major risk multiplier. Vitamin D deficiency is another big one. Low levels, especially during childhood, are tied to a 60% higher chance of developing MS. Smoking? It doesn’t just hurt your lungs-it speeds up disability progression by 80%. Genetics alone won’t give you MS. You need the right mix of genes and triggers. Even identical twins, who share 100% of their DNA, only have a 25% chance of both getting MS if one has it. So it’s not fate. It’s a perfect storm of biology and environment.The Real Symptoms: More Than Just Numbness
Most people think MS means losing the ability to walk. But the most common symptom? Fatigue. Eight out of ten people with MS describe it as overwhelming, unlike regular tiredness. It hits like a heavy blanket, making even simple tasks feel impossible. Vision problems come next. Optic neuritis-swelling of the optic nerve-is often the first sign. People report sudden blurring, pain when moving the eye, or loss of color vision. It can clear up in weeks, but the damage lingers. Numbness and tingling affect nearly 60% of patients. It’s not like a foot falling asleep. It’s persistent, sometimes crawling or burning. Walking becomes harder as muscles lose coordination. One in five people report bladder or bowel issues. Others get Lhermitte’s sign-a sharp electric shock down the spine when they bend their neck. It’s not dangerous, but it’s startling. And then there’s brain fog. Memory slips, trouble finding words, difficulty concentrating. These aren’t just stress-related. They’re direct results of inflammation in the brain’s gray matter, where thinking happens.
Two Main Types of MS-And What They Mean
About 85% of people start with relapsing-remitting MS (RRMS). They get flare-ups-attacks of new or worsening symptoms-followed by periods of recovery. These attacks can last days or weeks. Some people bounce back fully. Others are left with small deficits that pile up. The other 15% have primary progressive MS (PPMS). No flare-ups. No remissions. Just a slow, steady decline. Symptoms get worse over time, often starting with leg weakness or balance problems. PPMS is harder to treat because inflammation is less obvious. The damage is more about degeneration than active immune attacks. Over time, about half of RRMS patients transition to secondary progressive MS. The relapses fade, but the decline continues. This shift marks a change in the disease-from an immune-driven fire to a slow-burning embers of nerve death.How Treatments Fight Back
There’s no cure yet. But treatments have changed everything. Disease-modifying therapies (DMTs) don’t fix damaged nerves. They stop the immune system from attacking new ones. Ocrelizumab targets B cells. It’s the first drug approved for PPMS. In trials, it cut relapses by 46% in RRMS and slowed disability progression by 24% in PPMS. Natalizumab blocks immune cells from crossing the blood-brain barrier. It’s powerful-reducing relapses by 68%-but comes with a risk. One in a thousand people develop a rare brain infection called PML after long-term use. Newer drugs like siponimod and cladribine work differently, trapping immune cells in lymph nodes so they can’t reach the brain. Each has pros and cons. Side effects range from headaches to liver stress. The goal isn’t perfection-it’s stopping the attack before it causes more harm.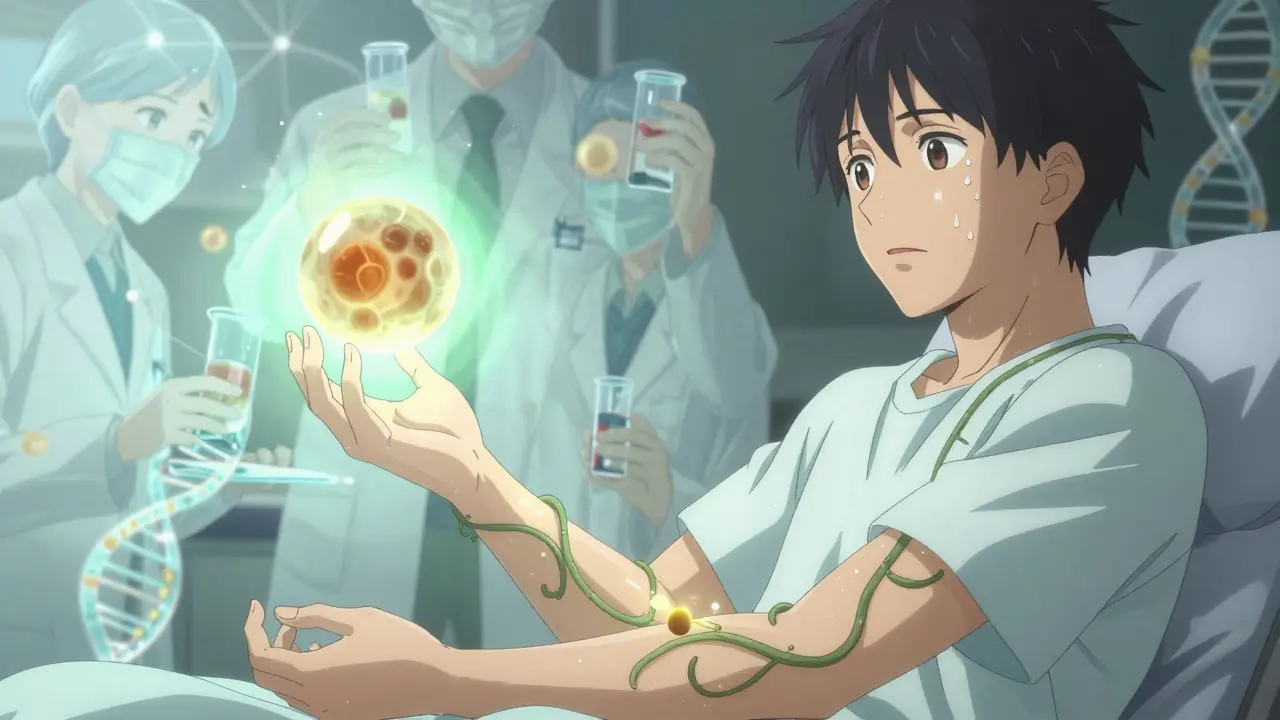
The Hope: Repairing What’s Broken
The biggest breakthroughs aren’t just about stopping damage-they’re about fixing it. Scientists used to think the brain couldn’t repair myelin. Now we know it can. Oligodendrocyte precursor cells are always trying to rebuild. But the inflammation around lesions creates a toxic environment. They can’t do their job. Clemastine fumarate, an old antihistamine, showed promise in early trials. It boosted remyelination in the optic nerve, improving signal speed by 35%. That’s not just a lab result-it means better vision, less fatigue, more function. Other drugs are being tested to wake up these repair cells. Some target specific proteins that block regeneration. Others use stem cells to replace lost oligodendrocytes. The International Progressive MS Alliance has poured $65 million into this research since 2014. Progress is slow, but real.What’s Next: Personalized Medicine
Future treatments won’t be one-size-fits-all. Blood tests now measure neurofilament light chain (sNfL). Levels above 15 pg/mL mean active inflammation is happening-even if you feel fine. That lets doctors adjust treatment before damage shows up on an MRI. Researchers are also tracking immune cell behavior in the spinal fluid. Specific dendritic cells are now known to carry myelin fragments to T cells, keeping the attack alive. Blocking those cells could stop the cycle. Neutrophil extracellular traps (NETs)-web-like structures released by immune cells-are found in 78% of MS relapses. They tear apart the blood-brain barrier. Targeting NETs could prevent attacks before they start. This isn’t science fiction. It’s happening now. Within five years, we’ll likely have blood tests that predict flare-ups, drugs that repair myelin, and treatments tailored to your immune profile.Living With MS Today
MS isn’t a death sentence. Life expectancy is close to normal for most. With modern treatments, 70% of people stay off assistive devices for 20 years or more. That’s a huge shift from the 1990s, when half of untreated RRMS patients needed a cane by age 40. Physical therapy, exercise, and stress management aren’t optional-they’re part of treatment. Yoga, swimming, and strength training help maintain mobility. A balanced diet and vitamin D supplements support overall health. Support matters too. Online communities like Reddit’s r/MS offer real stories: someone describing their first optic neuritis attack, another sharing how they learned to walk again after a relapse. These aren’t just stories-they’re lifelines. The immune system attacked. But medicine is fighting back-with science, with patience, and with hope.Comments (12)
-
Stephen Tulloch January 17, 2026
Bro this post is basically a Nobel Prize in neuroimmunology wrapped in a Reddit thread 🤯
My cousin got diagnosed last year and I swear she’s been living in a sci-fi novel since then. The fact that clemastine-a cheap antihistamine-can boost remyelination? That’s the kind of serendipity that makes science beautiful. Also, NETs? Neutrophil extracellular traps? I didn’t even know immune cells could make spider webs 😅
Who needs Marvel when we’ve got our own biological superheroes and villains?
-
Corey Sawchuk January 19, 2026
Been living with RRMS for 12 years. Fatigue is the real monster. Not the walking. Not the numbness. It’s the 3pm brain fog where even opening your eyes feels like lifting weights.
DMTs help, but nothing fixes that heavy blanket feeling. Still, I’m one of the lucky ones. Still drive. Still work. Still laugh.
Thanks for writing this. It’s rare to see the real stuff laid out like this.
-
Riya Katyal January 19, 2026
Oh so now it’s EBV’s fault? Next you’ll tell me my WiFi router caused my MS. 😏
My aunt had MS and she never even had mono. And she lived in Delhi. So much for ‘Scandinavian genetics’ lol.
Also, vitamin D? You think I’m gonna start taking supplements because some study says so? I’m not a lab rat.
-
Henry Ip January 20, 2026
This is one of the clearest explanations I’ve ever read. I’ve been reading up since my sister got diagnosed last year.
It’s wild how much we’ve learned in the last decade. The part about oligodendrocyte precursor cells trying to repair but getting drowned in inflammation? That’s heartbreaking and beautiful at the same time.
Keep sharing stuff like this. It helps families like mine feel less lost.
-
kanchan tiwari January 20, 2026
THEY KNOW. THEY’VE ALWAYS KNOWN.
Big Pharma is hiding the cure. Why do you think they’re pushing these $80,000/year drugs? Because they want you dependent. The real cure is turmeric, cold plunges, and avoiding 5G towers.
My cousin’s friend’s yoga teacher’s dog had MS and it vanished after she chanted mantras near its bed. Coincidence? I THINK NOT.
Also, why do all the researchers work for corporations? WHO IS PAYING THEM??
-
Bobbi-Marie Nova January 22, 2026
Okay but can we talk about how insane it is that an antihistamine might help repair nerves??
I mean, I use that stuff for my allergies and now I’m supposed to believe it’s secretly a neuro-repair wizard? 🤯
Also, I’m just here saying-people with MS are the real MVPs. You’re fighting a war inside your body and still showing up for life. I’m sending you all virtual tacos and hugs 🌮❤️
-
Allen Davidson January 23, 2026
Great breakdown. The part about PPMS being harder to treat because inflammation is less obvious? That’s the key. Most people think MS is just flares. But the slow burn? That’s the silent killer.
And yeah, the sNfL blood test? That’s going to change everything. Early detection before symptoms show up? That’s the future.
Keep pushing for research. We’re not there yet, but we’re closer than ever.
-
Ryan Hutchison January 24, 2026
Canada and Scandinavia have high rates? No wonder. Too much snow, too much vitamin D deficiency, too many weak genes.
Here in the US, we got real people. We don’t get MS because we eat real food, lift real weights, and don’t cry about everything.
Also, EBV? That’s just a virus. If you’re weak, you get sick. Simple as that.
-
Samyak Shertok January 24, 2026
So we’re told the immune system is betraying us... but isn’t that just nature’s way of pruning the unfit?
If evolution selected for people who survive MS, why are we trying to stop it?
Maybe the body isn’t broken. Maybe it’s trying to tell us something.
And what if myelin isn’t insulation... but a prison?
What if the real disease is our refusal to accept chaos?
Also, I’ve heard the real cause is electromagnetic radiation from smartphones. The WHO is covering it up.
Or maybe it’s the aliens. I mean, why else would it target the nervous system? They’re harvesting consciousness.
Just saying.
Also, I’m not saying any of this. I’m just asking questions. 😇
-
evelyn wellding January 26, 2026
Y’all are doing amazing. Seriously. I know it’s hard. I’ve been there. You’re not alone.
And guess what? You’re not just surviving-you’re teaching the world how to be brave.
Keep going. One step. One day. One breath. 💪❤️
Also, if you’re tired today, that’s okay. Rest is part of the fight. You’re still winning.
-
Chelsea Harton January 26, 2026
My cousin has MS and she said the worst part is people saying 'but you don’t look sick' like it's a compliment
Also clemastine is wild
and why is everyone so surprised that the brain can heal
it’s a body not a phone
we just forgot how to listen
-
Stephen Tulloch January 28, 2026
Wait wait wait-so if clemastine helps remyelination, and it’s an antihistamine...
does that mean allergies and MS are somehow connected?
Like... what if the immune system is just overworked from pollen and dust mites and then it snaps and starts attacking myelin?
That’s wild. I need to read more.
Also, I just Googled NETs and now I’m scared of my own neutrophils.
They’re out here making spiderwebs in my spinal fluid??
Y’all. I’m gonna go cry into my oat milk latte now.
