
When your kidneys aren’t working well, what you eat becomes just as important as any medication. A renal diet isn’t about losing weight or eating ‘clean’-it’s about protecting what’s left of your kidney function and avoiding dangerous imbalances in your blood. For people with stage 3 to 5 chronic kidney disease (CKD), managing sodium, potassium, and phosphorus isn’t optional. It’s life-preserving.
Why Sodium Matters More Than You Think
Sodium pulls water into your bloodstream. Healthy kidneys balance this by removing the extra fluid. But when kidneys fail, that fluid stays. The result? Swollen ankles, high blood pressure, shortness of breath, and extra strain on your heart. The goal isn’t to eliminate salt entirely-it’s to cut it back hard.The standard target for non-dialysis CKD patients is 2,000 to 2,300 milligrams per day. That’s about one teaspoon of table salt. Sounds simple? It’s not. Around 75% of the sodium people eat comes from packaged and restaurant foods, not the salt shaker. A single serving of canned soup can hit 1,200 mg. One slice of processed deli meat? 500 mg. A bag of flavored chips? Often over 300 mg.
Reading labels isn’t just helpful-it’s essential. Look for terms like “sodium,” “salt,” “monosodium glutamate (MSG),” and “baking soda.” Even “low-sodium” products can sneak in hidden salt. Instead of salt, use herbs: oregano, thyme, rosemary, or spice blends like Mrs. Dash. These add flavor without the risk. Cutting sodium by just 1,000 mg a day can drop systolic blood pressure by 5 to 6 mmHg, which reduces heart strain and slows kidney damage.
Potassium: The Silent Threat
Potassium helps your muscles and heart beat normally. But when your kidneys can’t filter it out, levels climb. A potassium level above 5.5 mEq/L can trigger dangerous heart rhythms-or even cardiac arrest. That’s why many CKD patients need to limit potassium to 2,000-3,000 mg per day, depending on their blood tests.Not all high-potassium foods are obvious. Bananas? 422 mg each. Oranges? 237 mg each. Potatoes? Over 600 mg in a medium one. Even tomatoes, spinach, and avocados pack a punch. But you don’t have to give them up entirely. Portion control and preparation matter.
Leaching vegetables can cut potassium by half. Slice potatoes, carrots, or beets thin, soak them in warm water for 2-4 hours, then boil them in plenty of water. Drain and rinse. That’s how DaVita Kidney Care recommends reducing potassium in veggies. Swap bananas for apples (150 mg each) or berries (65 mg per half cup). Choose cabbage (12 mg per half cup cooked) over spinach. And remember: potassium from animal sources-like meat, dairy, and fish-is absorbed more fully than from plants. So even if a food seems “healthy,” it might still be risky.
Phosphorus: The Hidden Killer in Processed Foods
Phosphorus is everywhere in your diet. But here’s the catch: your body absorbs almost all the phosphorus added to processed foods-90-100%. Natural phosphorus in foods like meat, dairy, and beans? Only 50-70% gets absorbed. That’s why two people eating the same amount of phosphorus can have wildly different blood levels.Colas? One 12-ounce can has 450 mg. Processed cheese? 250 mg per slice. Instant mashed potatoes? Up to 200 mg. Even some breads and cereals contain phosphorus additives labeled as “calcium phosphate” or “sodium phosphate.” These aren’t listed as “phosphorus” on labels, but they’re just as dangerous.
The recommended limit for non-dialysis CKD patients is 800-1,000 mg daily. That means swapping white bread (60 mg per slice) for whole grain (150 mg), choosing rice milk over cow’s milk (125 mg per half cup), and avoiding deli meats and frozen meals. Dairy is tricky-it’s a good source of protein but high in phosphorus. A small portion of cheese or milk is okay, but not daily. Egg whites are a better protein source than whole eggs-they’re lower in phosphorus and still packed with quality protein.
Real Food Swaps That Work
Changing your diet doesn’t mean eating bland, boring meals. It means making smarter choices. Here’s how real people do it:- Instead of orange juice, drink apple juice (lower potassium, no added phosphorus).
- Swap regular pasta for white rice noodles-less phosphorus, less potassium.
- Use lettuce wraps instead of whole wheat tortillas. One tortilla can have 100 mg phosphorus; a few lettuce leaves have none.
- Choose grilled fish like cod or halibut (low sodium, moderate potassium) over smoked salmon or canned tuna (high sodium, high phosphorus).
- Make your own broth using fresh herbs and vegetables instead of buying canned or powdered versions.
Many people struggle with flavor at first. Salt is addictive. But after a few weeks, your taste buds reset. You start noticing the natural sweetness in carrots, the earthiness in mushrooms, the brightness of lemon zest. It’s not deprivation-it’s recalibration.
Fluids and Protein: The Other Pieces
Fluid restriction often goes hand-in-hand with electrolyte management. If you’re making less than 1 liter of urine a day, your doctor may limit fluids to 32 ounces daily. That includes water, coffee, tea, soup, ice cream-even ice cubes. Track everything. A small cup of coffee counts. A half-slice of watermelon counts.Protein is another balancing act. Too much puts stress on your kidneys. Too little leads to muscle loss and weakness. The current standard? 0.55 to 0.8 grams of high-quality protein per kilogram of body weight. For a 70 kg person, that’s 38-56 grams per day. Egg whites, lean poultry, fish, and plant-based proteins like tofu (in moderation) are good choices. Avoid processed meats. They’re high in sodium, phosphorus, and preservatives.
What the Experts Say
Dr. Linda Fried from Columbia University says proper dietary management can delay dialysis by 6 to 12 months in stage 4 CKD patients. That’s a year of independence, fewer hospital visits, and better quality of life. Registered Dietitian Amy Meyer from the Cleveland Clinic points out that many patients fixate on potassium and miss the bigger picture: phosphorus additives are silently wrecking their health. “We see people eating salads with fresh veggies and drinking sparkling water, but they’re still on processed snacks and colas. That’s where the damage happens.” The European Renal Association argues that phosphorus limits below 1,200 mg/day may not improve survival in non-dialysis patients. But most U.S. guidelines stick with the 800-1,000 mg target because the risks of high phosphorus-bone fractures, heart calcification, and early death-are too real to ignore.
Tools and Support Are Out There
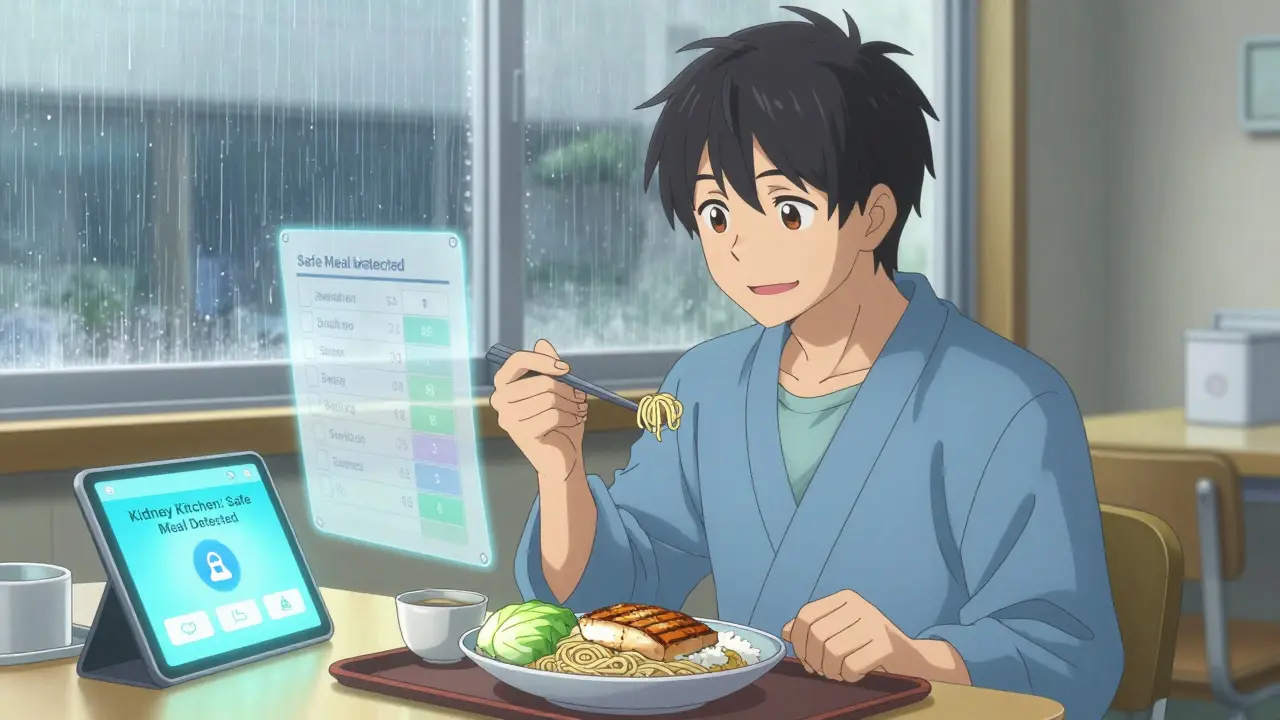
You don’t have to do this alone. Medicare now covers 3-6 sessions per year with a renal dietitian for stage 4 CKD patients. That’s free, personalized help. Apps like Kidney Kitchen let you scan barcodes and see sodium, potassium, and phosphorus levels in real time. Downloaded over 250,000 times, it’s one of the most trusted tools for people managing CKD. And new research is coming fast. The NIH’s PRIORITY study, launched in January 2024, is testing whether genetic tests can predict how your body handles potassium and phosphorus. Future apps may adjust your diet plan based on your latest lab results-automatically.What Not to Do
Don’t follow generic “healthy eating” advice if you have CKD. The Mediterranean diet? Great for most people-but full of potassium-rich tomatoes, nuts, beans, and potatoes. The DASH diet? Designed for high blood pressure, but it’s loaded with potassium and phosphorus. What’s heart-healthy for a 50-year-old might be dangerous for someone with stage 3 CKD. Don’t skip meals or restrict protein too much. A 2022 study found that elderly CKD patients on ultra-low protein diets had a 34% higher risk of malnutrition. You need enough protein to keep your muscles strong and your immune system working. Don’t assume “natural” means safe. Herbal teas, salt substitutes (often high in potassium), and “detox” cleanses can be risky. Talk to your dietitian before trying anything new.Final Thought: It’s a Lifeline, Not a Punishment
A renal diet isn’t about perfection. It’s about progress. Some days you’ll nail it. Other days, you’ll eat something that spikes your potassium. That’s okay. What matters is that you’re learning, adjusting, and staying in touch with your care team.People who stick with the diet live longer. They spend less time in the hospital. They keep their independence. And they feel better-less swollen, less tired, more in control.
You’re not just eating to survive. You’re eating to stay well.
Can I still eat fruits and vegetables on a renal diet?
Yes, but you need to choose wisely and prepare them correctly. Low-potassium options like apples, berries, cabbage, and green beans are safe in controlled portions. Avoid bananas, oranges, potatoes, tomatoes, and spinach unless you leach them first. Leaching-soaking sliced veggies in warm water for 2-4 hours, then boiling them in plenty of water-can reduce potassium by up to 50%. Portion size matters: a half-cup of cooked veggies is usually safer than a full cup.
Is sea salt or kosher salt better than table salt for a renal diet?
No. All types of salt-table salt, sea salt, kosher salt, Himalayan salt-are made of sodium chloride. They all contain the same amount of sodium per gram. Switching salt types won’t lower your sodium intake. The key is reducing total salt use, not changing the kind. Use herbs, spices, lemon juice, or salt-free blends instead.
Do I need to avoid dairy completely?
No, but you need to be careful. Milk, cheese, and yogurt are high in both phosphorus and potassium. A half-cup of milk has 125 mg of phosphorus. One slice of processed cheese can have 250 mg. If you enjoy dairy, choose small portions and opt for lower-phosphorus alternatives like rice milk or almond milk (check labels-some have added phosphorus). Egg whites are a great protein substitute if you’re cutting back on dairy.
Can I drink soda on a renal diet?
Most sodas are off-limits. Colas contain phosphoric acid, which adds about 450 mg of phosphorus per 12-ounce can-nearly half your daily limit. Even diet colas have the same phosphorus content. Sparkling water without additives is fine. Herbal teas (without added potassium) and water are your safest choices. Always check labels for hidden phosphorus additives like “phosphoric acid” or “sodium phosphate.”
How long does it take to adjust to a renal diet?
Most people need 3 to 6 months to fully adapt. The first few weeks are the hardest-your taste buds are used to salt, sugar, and strong flavors. But over time, you’ll start to appreciate the natural taste of food. Many patients say they feel better within weeks: less bloating, more energy, clearer thinking. Working with a renal dietitian makes the transition smoother and more sustainable.
Is a renal diet the same as a diabetic diet?
No, and that’s a common point of confusion. Many heart-healthy foods recommended for diabetics-like beans, nuts, whole grains, bananas, and oranges-are high in potassium or phosphorus and not safe for advanced CKD. Managing both conditions means finding a middle ground: choosing low-potassium carbs (like white rice instead of brown), limiting fruit portions, and avoiding processed foods that spike blood sugar and phosphorus at the same time. A dietitian can help you balance both needs safely.
Can I eat out at restaurants on a renal diet?
Yes, but you need to plan ahead. Ask for no added salt, no sauces or gravies, and grilled instead of fried. Avoid soups, salads with cheese or croutons, and dishes with processed meats. Request side dishes like steamed vegetables or plain rice. Many restaurants will accommodate these requests if you explain you have kidney disease. Apps like Kidney Kitchen can help you check nutrient content before you order.
What happens if I don’t follow the renal diet?
Ignoring the diet can lead to serious complications. Too much sodium causes fluid buildup, high blood pressure, and heart strain. High potassium can trigger irregular heartbeats or cardiac arrest. Excess phosphorus weakens bones, calcifies blood vessels, and increases the risk of heart disease. These issues can lead to hospitalization, faster progression to dialysis, or even early death. Following the diet isn’t about being perfect-it’s about protecting your health for as long as possible.
Sticking to a renal diet is one of the most powerful things you can do for your kidneys. It’s not easy, but it’s worth it. Every choice you make-from what’s on your plate to how you read a food label-adds up. You’re not just managing numbers. You’re protecting your body, your energy, and your future.
Comments (10)
-
Ryan W January 25, 2026
Let’s be real-this guide is just government-approved propaganda wrapped in medical jargon. 2,000 mg sodium? That’s a joke. My grandpa ate bacon and beans every day till he was 92. The real killer is pharmaceuticals, not salt. They’re milking this whole ‘renal diet’ scam to sell more meds and kidney monitors. Read the FDA’s own data-phosphorus additives are barely correlated with mortality. This is fearmongering dressed as science.
-
Allie Lehto January 26, 2026
OMG i just cried reading this 😭 i’ve been eating bananas every day thinking i was ‘healthy’ and now i feel like a monster… but also kinda free? like, finally understanding why my legs swelled up so bad after pizza night… i’m switching to apples and leaching my potatoes like a sacred ritual now 🙏✨ #renalawakening
-
Henry Jenkins January 26, 2026
I’ve been managing stage 4 CKD for 5 years and I appreciate the depth here, but there’s a critical gap: individual variability. The 800–1,000 mg phosphorus target assumes uniform absorption, but gut microbiome composition, gastric pH, and even vitamin D status drastically alter phosphorus bioavailability. One patient might tolerate 1,200 mg with normal serum levels while another hits 6.0 mEq/L on 700 mg. We need personalized biomarker tracking, not one-size-fits-all guidelines. Also, leaching works, but it’s labor-intensive-why isn’t there more research into enzymatic potassium reduction techniques? The food industry could innovate here if incentivized.
-
Dan Nichols January 27, 2026
Everyone’s obsessed with potassium but nobody talks about how dairy is the real silent killer. Milk has 370 mg phosphorus per cup. Cheese? 500+. And you think egg whites are better? They’re fine but still not magic. What about tofu? High in phytates which bind phosphorus-better than cheese. And why no mention of phosphate binders? If you’re eating processed food anyway, take a binder. Stop pretending diet alone fixes this. It’s a bandaid on a ruptured artery.
-
Renia Pyles January 27, 2026
You people act like this diet is some noble sacrifice. Newsflash-it’s torture. I miss salt. I miss cheese. I miss the taste of food. And now I’m supposed to feel grateful because I didn’t die yet? This isn’t living, it’s waiting. You think I want to eat boiled cabbage and rice noodles for the rest of my life? No. I want to eat a damn burger. And if I die from it? At least I died tasting something real.
-
George Rahn January 29, 2026
It is not merely dietary compliance that saves lives-it is the reclamation of agency in a system designed to commodify health. The American medical-industrial complex thrives on fear, on reductionism, on the illusion of control through quantified nutrients. But the true liberation lies in ancestral wisdom: whole foods, seasonal, unadulterated. The ancients did not measure phosphorus-they ate what the earth provided. We have forgotten that food is not data. It is communion. And in that communion, healing resides-not in the spreadsheet, but in the silence between bites.
-
Napoleon Huere January 29, 2026
What if the entire framework is wrong? We treat CKD like a mechanical failure-fix the numbers, fix the diet. But what if it’s an epigenetic signal? Chronic inflammation, stress, sleep deprivation-these are the true accelerants. Maybe we’re starving our bodies of adaptability by over-controlling food. I’ve seen patients thrive on higher protein, higher sodium diets when they reduced cortisol through meditation and circadian alignment. The kidneys aren’t broken-they’re overwhelmed. What if the real prescription isn’t a food log, but a life log? Sleep. Breath. Purpose. Maybe the real renal diet is learning how to stop fighting your body and start listening to it.
-
SWAPNIL SIDAM January 31, 2026
Brother, I am from India, we eat dal, rice, chapati-no salt, no processed stuff. My uncle has CKD, he eats boiled spinach, no tomato, no banana. He is alive at 78. You don’t need fancy apps. Just eat simple. God made food for us, not for labels. Less salt, less sugar, more prayer. That is the real diet.
-
Curtis Younker January 31, 2026
Y’all are overthinking this. I’ve been on this diet for 3 years and honestly? It’s not that bad once you get into a groove. I started with just swapping soda for sparkling water-game changer. Then I stopped buying pre-packaged meals. Made my own chicken broth with parsley and garlic-tastes amazing. I even started a little garden with lettuce and green beans. Feels good to grow your own food. You don’t have to be perfect. Just better than yesterday. And yeah, I still sneak a little cheese. But I track it. And I feel 10x better than I did 2 years ago. You got this.
-
Shweta Deshpande February 2, 2026
Reading this made me cry-not because I’m scared, but because I finally feel seen. I’ve been doing this alone for 4 years, afraid to ask for help. My husband thinks I’m being too strict. But now I know I’m not crazy. I’m fighting for my life. I’m going to book a session with a renal dietitian this week. And if you’re reading this and you’re scared-don’t be. You’re not alone. We’re all just trying to eat our way to tomorrow. One apple, one leached potato, one breath at a time. 💪❤️
