
More than 40% of adults taking prescription or over-the-counter meds are at risk of dangerous reactions when they drink alcohol. It’s not just about getting drunk faster. It’s about your heart, your liver, your breathing - and sometimes, your life.
How Alcohol Changes How Your Medications Work
Your liver doesn’t know the difference between alcohol and your medicine. Both are processed by the same enzymes - especially CYP2E1, CYP3A4, and CYP1A2. When you drink while on meds, these enzymes get overwhelmed. That’s when things go wrong.
There are two main ways this happens:
- Pharmacokinetic interactions: Alcohol changes how fast your body breaks down the drug. If you drink right after taking a pill, your body can’t process it properly. Blood levels of the drug can spike by 25% to 75% in under an hour. That’s like taking a double dose without knowing it.
- Pharmacodynamic interactions: Alcohol and the drug hit the same part of your body - like your brain or liver - and together, they amplify each other. This is especially dangerous with sedatives, painkillers, or antidepressants.
One study found that combining alcohol with benzodiazepines (like Xanax or Valium) boosts GABA activity in the brain by 400%. That’s not just drowsiness - it’s slowed breathing, loss of consciousness, or even death at very low alcohol levels - as little as 0.05% blood alcohol, which is just one drink for many people.
Medications That Can Kill You With Just One Drink
Some meds have interaction risks so high, even a single beer can land you in the ER.
Metronidazole (Flagyl) - used for infections - causes a disulfiram-like reaction in 92% of people who drink. Symptoms: flushing, pounding heart, nausea, vomiting, chest pain. One Reddit user wrote: “Had one beer with my Flagyl dose. Ended up in the ER with a heart rate of 180.” That’s not a myth. It’s documented in Infectious Diseases Society of America guidelines.
Benzodiazepines - like diazepam (Valium), alprazolam (Xanax), and lorazepam (Ativan) - are the most common cause of fatal alcohol-medication interactions. Alcohol makes these drugs last longer in your body. Diazepam’s half-life jumps from 20-100 hours to 35-150 hours when mixed with alcohol. That means the sedative effect sticks around way longer than you expect.
Opioids - including morphine, oxycodone, and hydrocodone - become 8 times more dangerous with alcohol. The CDC reports this combo is behind a growing number of overdose deaths. Both depress your breathing. Together, they can stop it completely.
Antidepressants - especially SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) - don’t cause fatal reactions, but they make alcohol hit harder and last longer. Studies show alcohol intoxication lasts 3.2 hours longer than normal. You feel more dizzy, more depressed, more out of control.
Antihistamines - like diphenhydramine (Benadryl) - are in many sleep aids and cold meds. With alcohol, their drowsiness effect triples. You could fall asleep behind the wheel or choke on your own saliva.
Over-the-Counter Meds Are Just as Dangerous
You don’t need a prescription to get hurt.
Acetaminophen (Tylenol) - the most common painkiller in the U.S. - can cause sudden liver failure if you drink regularly. The FDA warns against more than 3 drinks a day with acetaminophen. But a 2023 Hepatology study found that even moderate drinking - just one or two drinks daily - raised liver enzyme levels in 45% of people taking standard doses. Your liver doesn’t scream before it fails.
NSAIDs - like ibuprofen (Advil), naproxen (Aleve), and aspirin - increase your risk of stomach bleeding by 300% to 500% when mixed with alcohol. That’s not just an upset stomach. That’s internal bleeding that can require surgery.
Who’s at Highest Risk?
It’s not just about how much you drink. It’s about who you are.
Older adults - especially those over 65 - process alcohol and meds slower. Liver blood flow drops by 35% between ages 25 and 75. The American Geriatrics Society lists 17 medications with dangerous alcohol interactions for seniors. Many are prescribed for sleep, pain, or anxiety - exactly the kinds of drugs people reach for at night.
People taking 5 or more meds - nearly 70% of adults over 65 do. More drugs = more chances for alcohol to interfere. One study found 68% of people in this group have no idea their meds interact with alcohol.
People who drink daily - even if it’s just one glass of wine - train their liver to break down alcohol faster. That means your meds get cleared out too quickly. You might think your painkiller isn’t working, so you take more. That’s how accidental overdoses happen.
What You Can Do Right Now
You don’t need to be a doctor to protect yourself. Here’s what works:
- Ask your pharmacist - every time you pick up a new prescription. Pharmacists are trained to spot these interactions. Walgreens found that 89% of patients changed their drinking habits after getting a simple warning from a pharmacist.
- Check your meds - Look at the bottle. Is there a warning about alcohol? Only 42% of prescription labels include it, according to the FDA. Don’t rely on the label. Ask.
- Know your standard drink - 12 oz beer (5% ABV), 5 oz wine (12% ABV), or 1.5 oz spirits (40% ABV) = one drink. Anything more is a risk.
- Wait 72 hours - If you’re starting metronidazole, tinidazole, or disulfiram, don’t drink for 3 full days before and after. That’s the only way to avoid the life-threatening reaction.
- If you drink, wait 2-3 hours after taking your pill - and eat food first. Food slows alcohol absorption by 25-30%.
- Limit to one drink - for women, or two for men - if you must drink with meds that aren’t high-risk. Even then, watch for dizziness, nausea, or confusion.
Why Doctors Don’t Always Warn You
Only 32% of doctors routinely ask patients about alcohol use during visits. A 2022 AARP survey found 68% of patients were never told about alcohol-medication risks. Why?
- Time constraints - a 15-minute visit doesn’t leave room for deep conversations.
- Assumptions - many doctors assume patients won’t drink, or won’t admit it.
- Outdated info - some providers still think “one glass of wine is fine” with most meds, even though evidence says otherwise.
But things are changing. Starting in January 2024, the FDA requires new warning labels with pictograms on high-risk medications. Telehealth platforms now use screening tools like the AUDIT-C questionnaire to catch risky drinking before prescriptions are written.
What’s Next for Patient Safety
Technology is catching up. Stanford Medicine tested an AI system that flagged dangerous alcohol-medication combos in electronic health records. In six months, inappropriate combinations dropped by 37%.
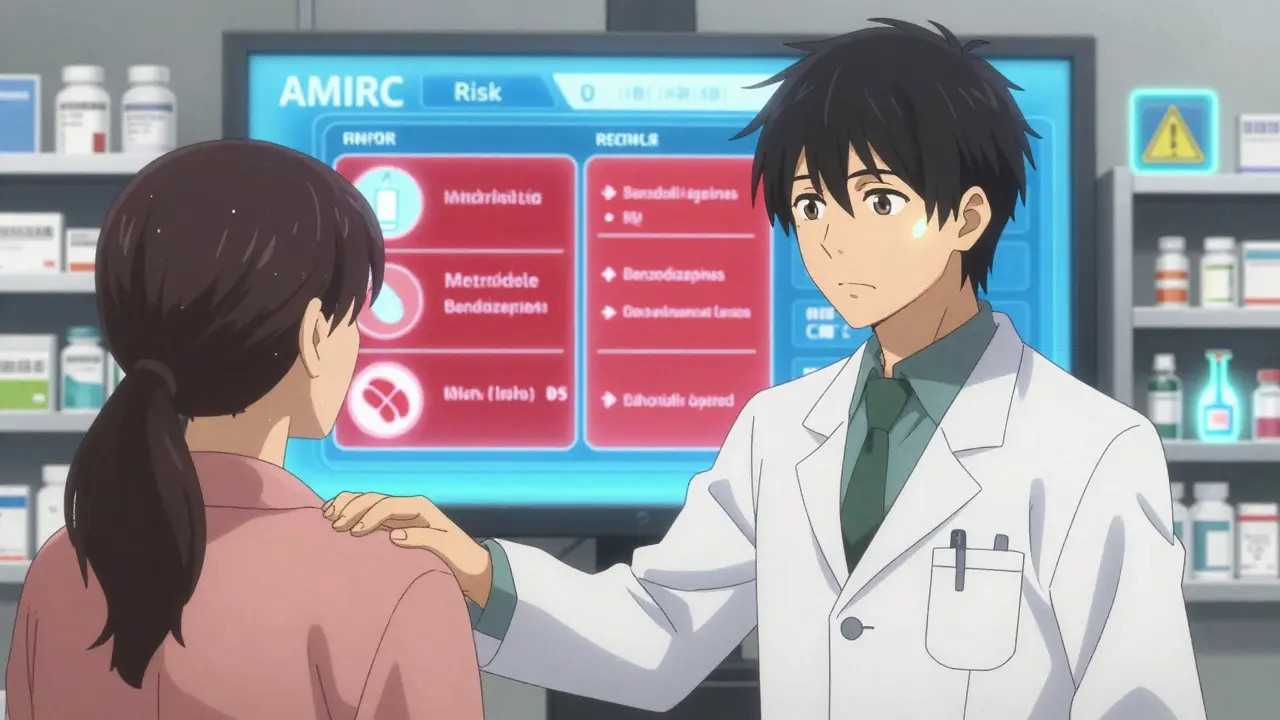
The NIAAA now offers a free online tool called the Alcohol-Medication Interaction Risk Calculator (AMIRC). You plug in your meds, your drinking habits, your age, and your liver health - and it gives you a personalized risk score.
But tools won’t help if you don’t know they exist. That’s why education matters more than ever.
Real Stories, Real Risks
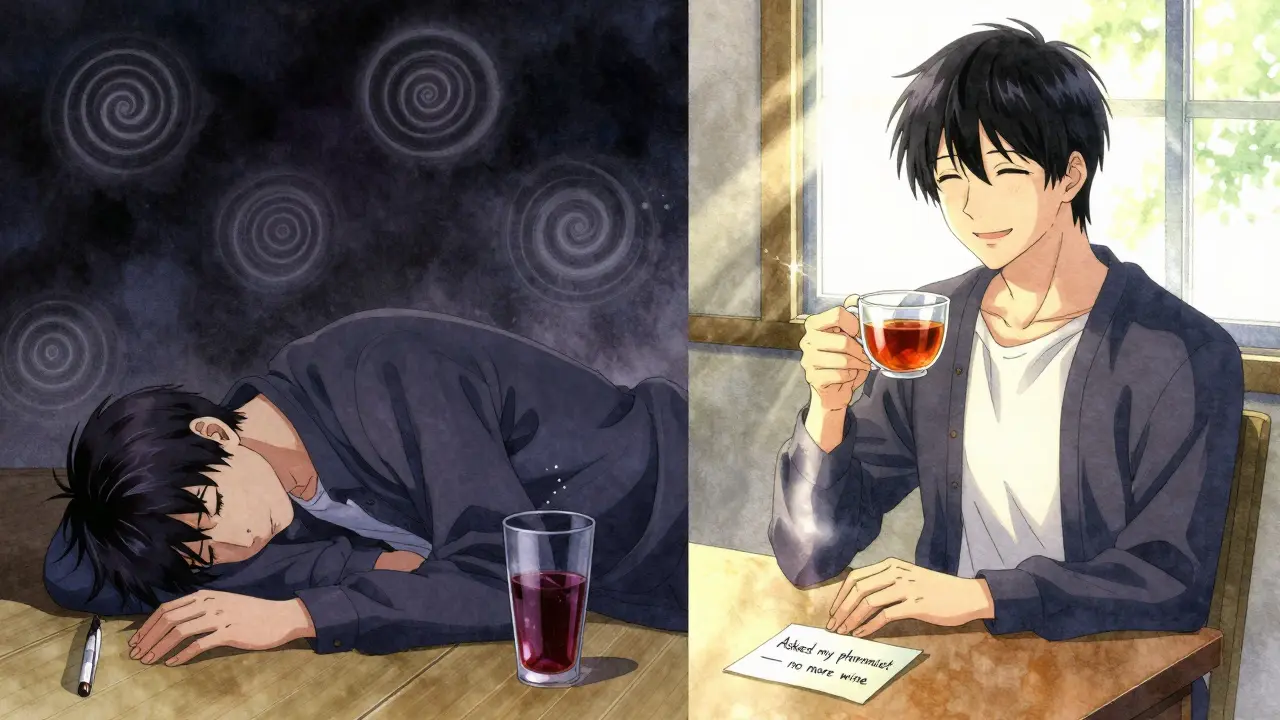
On Reddit, a man wrote: “I took my hydroxyzine for anxiety, had a glass of wine at dinner. Woke up on the floor. Couldn’t remember how I got there.”
Another said: “My pharmacist told me not to drink with my amitriptyline. I didn’t believe her. Had a beer. Felt like I was falling through the floor. Took me 3 days to feel normal again.”
These aren’t rare. Drugs.com has over 78,000 user reports of bad reactions. Top offenders: alprazolam, amitriptyline, and warfarin.
But there are wins too. One woman said: “My pharmacist warned me about mixing my blood pressure med with wine. I cut it out. My BP dropped 20 points. I didn’t even know it was the alcohol.”
Final Thought: It’s Not About Giving Up Drinking
It’s about staying in control.
You don’t have to quit alcohol forever. But if you’re on meds - especially for sleep, pain, anxiety, or infection - you need to know the rules. A single drink can turn a routine night into an emergency. A missed warning can cost you your health.
Ask. Check. Wait. Limit. These four steps could save your life.
Can I have one drink with my medication?
It depends on the medication. For some - like metronidazole, benzodiazepines, or opioids - even one drink is dangerous. For others - like most SSRIs or NSAIDs - one drink may be okay if you’re healthy and don’t drink often. But there’s no universal safe level. Always check with your pharmacist or doctor before drinking.
How long should I wait after taking my medication before drinking?
For high-risk meds like metronidazole, wait 72 hours before and after. For others, wait at least 2-3 hours after taking your dose. But timing alone isn’t enough. Alcohol stays in your system for hours, and some meds stay in your body for days. If you’re unsure, don’t risk it.
Does alcohol make all medications less effective?
No. Sometimes it makes them stronger. Chronic alcohol use can make your liver break down meds faster, reducing their effect. But acute drinking - like having a drink with your pill - usually slows down metabolism, making the drug stronger. That’s why you might feel overly drowsy or dizzy after just one drink.
Is it safe to drink alcohol while taking antibiotics?
Most antibiotics - like amoxicillin or azithromycin - don’t interact badly with alcohol. But metronidazole, tinidazole, and linezolid can cause severe reactions. Always check the label or ask your pharmacist. Don’t assume all antibiotics are safe.
Can alcohol affect my blood pressure meds?
Yes. Alcohol can make blood pressure meds work too well, causing dizziness or fainting. It can also raise your blood pressure over time, making the meds less effective. If you’re on these meds, limit alcohol to one drink occasionally - and monitor how you feel.
Why do I feel more drunk on medication than usual?
Many meds - especially antidepressants, antihistamines, and sleep aids - slow down how your brain processes alcohol. That means you feel the effects faster and stronger. You might think you’re only having one drink, but your body treats it like two or three.
What should I do if I accidentally mixed alcohol with a risky medication?
If you feel dizzy, nauseous, have chest pain, trouble breathing, or your heart is racing - call emergency services immediately. Don’t wait. These reactions can escalate quickly. If you’re unsure, call poison control (1-800-222-1222 in the U.S.) or go to the nearest ER.
Comments (8)
-
Sahil jassy December 19, 2025Been there done that. Took Flagyl and had one beer. Heart racing like a drum machine. ER visit. Don't be stupid. 🚨
-
Dorine Anthony December 21, 2025This is so important. My grandma didn't know her blood pressure med and wine were fighting each other. She started feeling dizzy all the time. Once her pharmacist told her, her numbers improved overnight. 💯
-
Ryan van Leent December 22, 2025Yall act like alcohol is poison but i drink whiskey with my oxycodone every friday and im fine. Stop scaremongering. If you cant handle a drink and a pill you probably shouldnt be on pills
-
shivam seo December 24, 2025This is why Americans are so weak. In Australia we drink with antibiotics, painkillers, whatever. You get used to it. Your liver gets stronger. This fear-based medical nonsense is why your life expectancy is falling. One drink? Please.
-
benchidelle rivera December 25, 2025The data presented here is unequivocal. The pharmacokinetic and pharmacodynamic interactions between ethanol and central nervous system depressants are well-documented in peer-reviewed literature. To disregard this is to endanger not only oneself but others in one's vicinity. Please consult your pharmacist. This is not optional. Your life is not a gamble.
-
Anna Sedervay December 25, 2025I've noticed that the FDA's new pictogram warnings are being rolled out... but have you ever wondered if Big Pharma is actually *encouraging* this confusion? After all, if you're mixing meds with alcohol and ending up in the ER, you'll need more prescriptions... and more visits... and more $$$ for the system. The real danger isn't the alcohol. It's the profit motive behind the silence.
-
Dev Sawner December 26, 2025The statistical correlation between alcohol consumption and adverse drug reactions is not causal without controlling for confounding variables such as age, polypharmacy, and hepatic metabolism. Moreover, the cited Reddit anecdotes constitute anecdotal evidence, not empirical data. One must exercise epistemic rigor before drawing public health conclusions.
-
Moses Odumbe December 26, 2025Just got my new script for Zoloft. Pharmacist said 'one glass of wine is fine' 😌. So I did. Felt like I was underwater for 4 hours. My dog looked at me like I was a ghost. 🐶😵💫 Now I wait 4 hours after my pill. No more fun. But I'm alive.
