When someone is stuck in a deep, heavy depression, it’s easy to assume it’s just unipolar depression. But what if it’s not? What if that same depression is actually part of something bigger - bipolar depression - and treating it the wrong way could make things worse? This isn’t just academic. Misdiagnosing bipolar depression as unipolar depression happens in nearly 4 out of 10 cases, and the consequences can be life-altering.
What’s the Real Difference?
Unipolar depression, also called Major Depressive Disorder (MDD), means you experience depressive episodes - low mood, no energy, trouble sleeping, loss of interest - but you’ve never had a manic or hypomanic episode. That’s it. No highs. Just lows. Bipolar depression is different. It’s the low phase of bipolar disorder. People with bipolar disorder swing between depression and mania (or hypomania). Mania isn’t just feeling happy. It’s racing thoughts, little need for sleep, impulsive spending, risky behavior, or feeling invincible. Hypomania is milder but still noticeable - and it’s enough to change everything about how you treat the depression. The DSM-5, the standard diagnostic guide used by psychiatrists, makes this distinction clear: if you’ve ever had a manic or hypomanic episode, even once, your depression is part of bipolar disorder. Not unipolar. Not just "bad depression." Bipolar.How Doctors Tell Them Apart
It’s not always obvious. Many people with bipolar disorder first seek help during a depressive episode. They don’t mention the highs because they don’t see them as a problem. Maybe they even enjoyed them. That’s why doctors need to ask the right questions. Key red flags include:- Depression started before age 25
- Multiple depressive episodes in a short time
- Depression that didn’t respond to two or more antidepressants
- Family history of bipolar disorder or suicide
- Psychotic symptoms during depression - like hearing voices or believing you’re being watched
- Early morning waking, severe fatigue, or feeling worse in the morning
- History of "switching" - feeling energized, irritable, or overly confident after starting an antidepressant
Why Treatment Can’t Be the Same
This is where things get dangerous. For unipolar depression, antidepressants like sertraline or escitalopram are the first-line treatment. About 60-65% of people respond within 8 to 12 weeks. But for bipolar depression? Antidepressants alone are a gamble. The STEP-BD study found that when people with bipolar disorder were treated with antidepressants without a mood stabilizer, 76% had their mood destabilized - meaning they cycled into mania, hypomania, or rapid cycling. That’s not a side effect. That’s a treatment failure. Instead, first-line treatments for bipolar depression are mood stabilizers and atypical antipsychotics:- Lithium - one of the oldest treatments, still effective. It reduces suicide risk and helps prevent future episodes. Response rate: 48% vs. 28% for placebo.
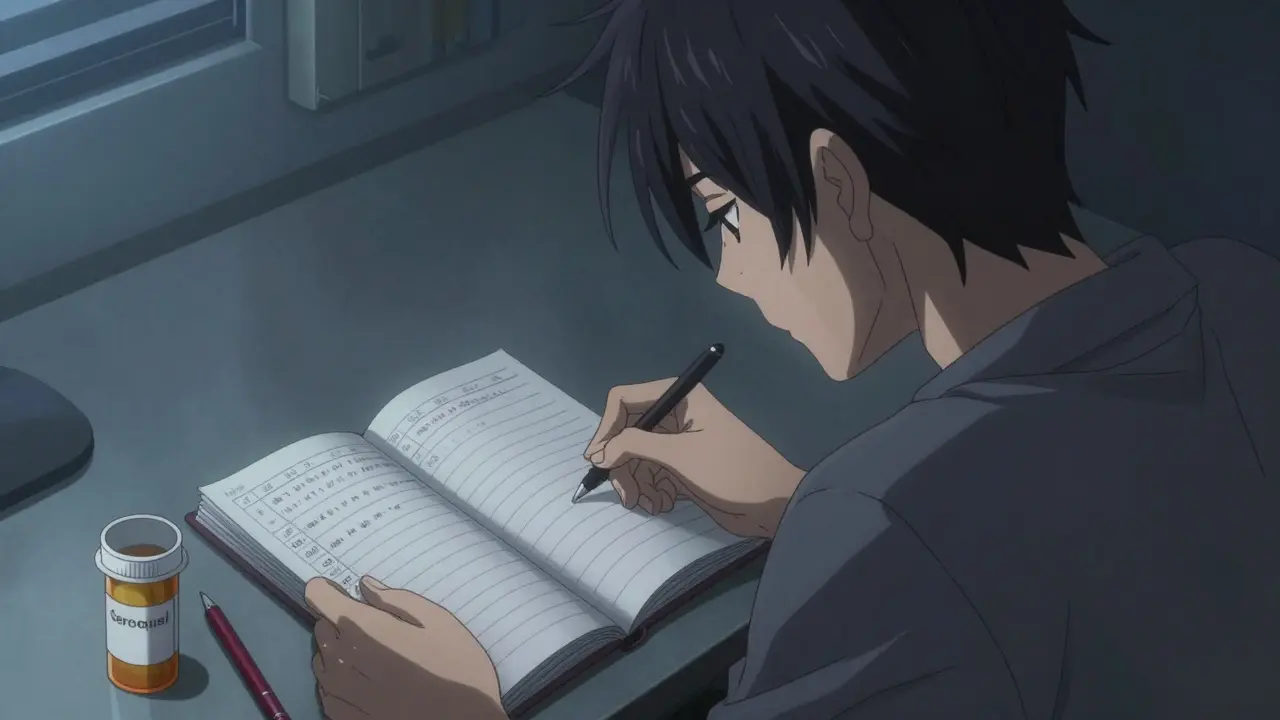
- Quetiapine (Seroquel) - approved specifically for bipolar depression. Response rate: 58% vs. 36% for placebo.
- Lurasidone (Latuda) - another FDA-approved option. Works well without causing weight gain.

Therapy Changes Too
Cognitive Behavioral Therapy (CBT) helps both types. But for unipolar depression, it’s mostly about changing negative thoughts. For bipolar depression, therapy has to be more structured around rhythm and stability. Interpersonal and Social Rhythm Therapy (IPSRT) focuses on keeping daily routines steady - sleep, meals, work, exercise. Why? Because disruptions in routine can trigger mood episodes. Studies show people using IPSRT have 68% remission rates after a year, compared to 42% with standard care. For bipolar disorder, therapy isn’t just about feeling better. It’s about preventing the next episode before it starts.The Hidden Risk: Antidepressants Triggering Mania
One of the most shocking truths? Many people with bipolar disorder were misdiagnosed for years - and treated with antidepressants the whole time. A 2017 study found that people with undiagnosed bipolar disorder spent an average of 8.2 years on the wrong treatment. During that time, 63% had at least one hospitalization because the antidepressant pushed them into mania. Reddit communities like r/bipolar are full of stories like this: > "I was on Prozac for 7 years. My psychiatrist said I had severe depression. I cycled from 2 episodes a year to 12. I lost my job. My marriage nearly ended. When they finally realized I had bipolar II, I was put on lithium - and everything changed." That’s not rare. The National Comorbidity Survey found that 40% of people with bipolar disorder were first diagnosed with unipolar depression. And 90% of them were given antidepressants alone.What Happens After Diagnosis?
Long-term management is where the divide gets wider. For unipolar depression, if you’ve had one episode and respond well, you might stop medication after 6 to 12 months of being symptom-free. Many people do. For bipolar disorder? Stopping medication is risky. About 73% of people relapse within five years if they stop their mood stabilizer. That’s why most people with bipolar disorder stay on medication for life - not because they’re "broken," but because it’s medical management, like insulin for diabetes. And relapse isn’t just feeling down. It can mean psychosis, hospitalization, job loss, or suicide.New Hope on the Horizon
Treatment is evolving. In 2019, the FDA approved esketamine nasal spray (Spravato) for treatment-resistant unipolar depression. It works fast - some feel better in hours. But it’s not approved for bipolar depression yet. For bipolar depression, cariprazine (Vraylar) got FDA approval in 2019. It’s a newer antipsychotic that targets dopamine receptors and showed better remission rates than placebo. Even more exciting? Research into biomarkers. A 2023 Lancet study identified a 12-gene pattern that can distinguish bipolar from unipolar depression with 83% accuracy. We’re not there yet for routine use, but it’s a step toward objective testing - not just relying on patient recall. Digital tools are also emerging. Apps that track sleep, speech patterns, and typing speed can detect subtle mood shifts before the person even notices them. This could help catch early signs of a switch - and prevent a full episode.What Should You Do If You’re Not Sure?
If you’ve been diagnosed with unipolar depression but:- Antidepressants didn’t help, or made things worse
- You’ve had periods of high energy, impulsivity, or irritability
- Family members have bipolar disorder
- You’ve had psychotic symptoms during depression
Why This Matters
This isn’t just about labels. It’s about survival. Getting the wrong treatment can cost you years - your job, your relationships, your safety. The economic cost? Over $13,000 more per year for misdiagnosed patients due to hospital stays and medication changes. But get it right? The difference is dramatic. People on the correct treatment report 52% fewer hospitalizations and 47% better work performance. Bipolar depression and unipolar depression look similar on the surface. But under the hood, they’re different machines. You wouldn’t put diesel in a gasoline engine. Don’t treat bipolar depression like unipolar. The stakes are too high.Can you have bipolar depression without ever having mania?
No. By definition, bipolar depression only occurs in people who have had at least one manic or hypomanic episode. If you’ve never had a high, your depression is classified as unipolar (Major Depressive Disorder). But many people don’t recognize hypomania - it can feel like being "on top of the world," super productive, or unusually confident. That’s why doctors ask about past energy levels, sleep needs, and risky behavior.
Are antidepressants ever safe for bipolar depression?
Only when used alongside a mood stabilizer like lithium or lamotrigine. Using antidepressants alone in bipolar disorder carries a high risk of triggering mania, rapid cycling, or worsening mood swings. Even then, they’re not first-line. They’re used only if the person still has depressive symptoms after mood stabilizers have done their job.
How long does it take to get the right diagnosis?
On average, it takes 8 to 10 years for someone with bipolar disorder to get the correct diagnosis. Many are misdiagnosed with unipolar depression, anxiety, or even personality disorders. The delay happens because people don’t report their highs, and doctors don’t always ask the right questions. If depression doesn’t respond to two antidepressants, bipolar should be considered.
Can bipolar depression turn into unipolar depression?
No. Once someone has had a manic or hypomanic episode, they have bipolar disorder for life. They may go long periods without mania, but the diagnosis doesn’t change. Some people with bipolar disorder have mostly depressive episodes and rarely experience mania - this is called bipolar II. But it’s still bipolar disorder. The diagnosis is based on history, not current symptoms.
What’s the best way to track my mood at home?
Use a simple mood journal. Each day, rate your mood from 1 to 10, note your sleep hours, and record any unusual behaviors - like spending too much money, talking faster than usual, or feeling unusually irritable. Apps like Daylio or eMoods can help. Bring this journal to appointments. It gives your doctor objective data instead of relying on memory.
Comments (10)
-
dean du plessis December 27, 2025
Been there. Got the t-shirt. Antidepressants made me feel like a robot on a rollercoaster. Then I got diagnosed with bipolar II and started on lamotrigine. Life didn’t just improve-it became something I actually wanted to live. No drama. Just quiet stability.
-
Miriam Piro December 29, 2025
Let’s be real-Big Pharma doesn’t want you to know the truth. They profit off endless prescriptions of SSRIs, but if you’re bipolar, those drugs are basically chemical triggers for mania. The DSM-5? A corporate tool. The real diagnosis? Your body screaming after 7 years of Prozac and 3 hospitalizations. They don’t test your brain-they test your wallet. And don’t get me started on how psychiatrists ignore hypomania because ‘it felt good’ 😤
My ex said I was ‘too intense’ during my highs. Turns out I was hypomanic. I maxed out three credit cards, quit my job to start a crypto empire, and drove 12 hours to ‘save’ a stranger I met on Reddit. All while thinking I was ‘inspired.’ Now I’m on lithium. My bank account’s recovering. My sanity? Still fragile. But I’m alive. And I know the system is rigged.
They call it ‘mental illness.’ I call it a malfunctioning system that rewards misdiagnosis. Why? Because treating bipolar right costs less money. And money talks louder than truth. 🤑🧠
Ask your doctor: ‘Have you ruled out bipolar?’ If they hesitate? Find someone new. Your life isn’t a clinical trial.
And yes-I still track my mood in a journal. And yes-I still cry sometimes. But now I know why. And that’s power.
They told me I was ‘just depressed.’ I told them I’d been ‘too awake’ for weeks. They laughed. Now they’re paying for my therapy. 💸
-
Kylie Robson December 31, 2025
From a neuropsychopharmacology standpoint, the differential diagnostic challenge stems from phenotypic overlap in monoaminergic dysregulation, particularly in serotonergic and dopaminergic pathways. The absence of a prior manic episode in clinical history is a critical exclusion criterion per DSM-5, yet retrospective recall bias-especially regarding hypomanic episodes-introduces significant diagnostic sensitivity error. The HCL-32 demonstrates superior psychometric properties for detecting subthreshold manic symptoms, with a reported sensitivity of 69% in bipolar II populations compared to the MDQ’s 28%. Antidepressant monotherapy in bipolar depression is contraindicated due to the high risk of treatment-emergent affective switch (TEAS), with STEP-BD data indicating a 76% destabilization rate. Lithium remains first-line due to its unique anti-suicidal and neuroprotective effects mediated via GSK-3β inhibition and BDNF upregulation. Quetiapine and lurasidone offer favorable side effect profiles with minimal metabolic burden, making them preferable in comorbid obesity or metabolic syndrome. The emerging 12-gene biomarker signature from the 2023 Lancet study represents a paradigm shift toward objective, neurobiologically grounded diagnostics-potentially rendering subjective symptom reporting obsolete within the next decade.
-
Caitlin Foster December 31, 2025
WAIT-so you’re telling me I was on antidepressants for 5 years and I was BIPOLAR the whole time?!?!?!?!?!!??!?!?!
MY LIFE WAS A LIE!!!
I thought I was just ‘a creative mess’-turns out I was a walking time bomb with a credit card and a Spotify playlist called ‘I’m Not Depressed, I’m Just Intense.’
And now I’m on lithium? And I don’t feel like a zombie? AND I’M SLEEPING?!?!?!?!?
Why didn’t anyone tell me this before?!?!?!?!
Also-my therapist is a genius. I’m crying. But good tears. 🥹
PS: If you’re reading this and on SSRIs and still feel like you’re drowning? ASK FOR A BIPOLAR SCREEN. I’m begging you. Your future self will send you a thank-you note.
-
Todd Scott January 1, 2026
I’ve worked in community mental health across six states, and I’ve seen this pattern over and over: someone comes in depressed, says they’ve never felt ‘high,’ but when you dig-there’s the one week in college where they didn’t sleep for five days, wrote a novel, and bought a motorcycle on impulse. Or the time they spent $8,000 on art supplies because ‘the universe told me to.’
Those aren’t personality quirks. Those are hypomanic episodes. And they’re often forgotten because they felt good. People don’t report them unless you ask specifically: ‘Have you ever had a time when you felt unstoppable, even if it ended badly?’
It’s not about stigma. It’s about framing. We need to normalize asking about highs, not just lows.
And yes-family history matters. If your mom had bipolar, your depression isn’t ‘just depression.’ It’s a red flag. Don’t wait for six episodes. Get screened early.
Also-mood journals are underrated. Even a sticky note with ‘sleep: 4hrs, spent $500, felt invincible’ can change everything.
-
Andrew Gurung January 1, 2026
Oh, so now we’re treating mental illness like it’s a car engine? Diesel in a gas tank? How… quaint. You think this is about biology? No. It’s about control. The psychiatric industrial complex needs you dependent. Lithium? Cheap. Effective. Unpatentable. So they push SSRIs-$120/month, lifelong, with side effects that make you forget your own name. Meanwhile, your ‘bipolar’ diagnosis is just a label to keep you quiet. They don’t want you to heal. They want you to pay. And if you’re lucky? You’ll live long enough to see them patent the next miracle drug. 💸
Meanwhile, I’m on lithium. And I’m not ‘cured.’ I’m just not being exploited anymore. 🤡
-
Paula Alencar January 2, 2026
It is of the utmost importance that we approach this subject with the gravity and compassion it so profoundly deserves. The misdiagnosis of bipolar depression as unipolar depression is not merely a clinical oversight-it is a systemic failure of empathetic inquiry, one that has left countless individuals stranded in the abyss of pharmaceutical trial and error, often for over a decade. The consequences are not merely statistical; they are human. They are the loss of careers, the dissolution of familial bonds, the erosion of self-worth, and, in too many cases, the irreversible tragedy of suicide. We must, as a society, demand more rigorous screening protocols, more comprehensive patient education, and above all, a cultural shift that recognizes mental health not as a moral failing, but as a biological reality requiring nuanced, individualized, and long-term care. To treat bipolar depression as if it were unipolar is not merely incorrect-it is an ethical violation of the highest order. Let us not be the generation that looked away.
-
Nikki Thames January 3, 2026
You say you ‘didn’t know’ you were hypomanic? That’s not ignorance. That’s denial. You enjoyed the highs. You thrived on the chaos. You thought it was ‘being your best self.’ But you didn’t see the wreckage-your relationships, your finances, your sleep schedule. You didn’t want to see it. Because facing it means admitting you’re not special-you’re sick. And that’s terrifying. But here’s the truth: you’re not broken because you have bipolar disorder. You’re broken because you refused to face it. And now you’re blaming the system. The system didn’t make you manic. You did. And now you’re lucky enough to be on lithium. So stop whining. Start taking responsibility.
-
Will Neitzer January 3, 2026
I appreciate the depth of this post and the emphasis on longitudinal care. One point that deserves amplification: the 73% relapse rate upon discontinuation of mood stabilizers is supported by long-term cohort studies from the Harvard Bipolar Program and the STEP-BD trial. It is not a matter of ‘lifelong medication’ as a punitive measure, but rather a neurobiological imperative-similar to thyroid hormone replacement or insulin therapy in type 1 diabetes. The brain’s circadian and monoaminergic regulatory systems in bipolar disorder exhibit persistent dysregulation, even during euthymia. Therefore, prophylactic pharmacotherapy is not a sign of weakness-it is a form of neuroprotective maintenance. Additionally, the integration of IPSRT with pharmacotherapy yields statistically significant improvements in relapse latency and functional recovery. This is evidence-based medicine, not ideology. We owe it to patients to provide the full spectrum of care, not just the easiest path.
-
Janice Holmes January 4, 2026
Okay-so I’ve been on lithium for 3 years now. And I’ll be honest-I thought I’d hate it. I thought I’d feel like a robot. But here’s the thing: I feel like ME. Not the version of me that cried for three days straight. Not the version that spent $10k on a yacht I didn’t need. Not the version that thought I could fly. I feel… calm. Clear. Human.
And the worst part? I didn’t even know I was missing it.
My mom cried when I told her I was bipolar. She said, ‘I always knew you were different.’
Turns out… we’re the same.
