
Birth control pills are one of the most common ways women prevent pregnancy-but they’re not as simple as just popping a pill every day. The difference between perfect use and typical use can mean the difference between 99% effectiveness and just 93%. That’s not a small gap. It’s 7 out of every 100 women getting pregnant in a year because they missed a pill, took it late, or didn’t know about a drug interaction. If you’re considering birth control pills, you need to know what really happens in your body, what can go wrong, and what might make them stop working-even if you think you’re doing everything right.
How Effective Are Birth Control Pills?
On paper, birth control pills are nearly perfect. With perfect use-taking the pill at the same time every single day, without missing a single dose-less than 1 in 100 women will get pregnant in a year. That’s 99% effective. But real life doesn’t work like that. People forget. People travel. People get sick. People take antibiotics or herbal supplements without thinking twice.
In real-world use, the number drops to about 93% effective. That means 7 out of every 100 women using the pill will get pregnant within a year. That’s not because the pill is broken. It’s because it’s easy to mess up. Compare that to an IUD or implant, which are over 99% effective even if you forget they exist. The pill doesn’t care how busy you are. It needs you to be consistent.
Younger women are especially at risk. Studies show women under 21 using the pill are almost twice as likely to experience an unintended pregnancy compared to women over 21. Why? Because younger users are more likely to miss doses or take pills late. It’s not about willpower-it’s about routines. If you don’t have a daily habit tied to brushing your teeth or eating breakfast, you’ll forget.
And here’s something most people don’t realize: the pill doesn’t start working right away. If you start on the first day of your period, you’re protected immediately. But if you start later, you need to use condoms or avoid sex for at least seven days. Skipping that step is a common reason for accidental pregnancy.
Two Types of Pills-And They Work Differently
Not all birth control pills are the same. There are two main types: combined pills and progestin-only pills (also called mini-pills).
Combined pills contain estrogen and progestin. Most modern versions have between 20 and 35 micrograms of estrogen-far less than the original 1960s pills, which had over 10,000 micrograms. That’s why today’s pills are safer. The most common and safest combination is 30 micrograms of ethinyl estradiol with levonorgestrel. These are the go-to for most doctors because they balance effectiveness with lower risk of blood clots and other side effects.
Progestin-only pills (POPs) contain no estrogen. They’re usually prescribed for women who can’t take estrogen-like those with a history of blood clots, migraines with aura, or who are breastfeeding. These pills are trickier. You have to take them at the exact same time every day, within a 3-hour window. Miss that window, and your protection drops fast. One study showed that missing a POP by just 3 hours increases pregnancy risk by 10 times compared to perfect use.
Newer POPs like Slynd® use a higher dose of drospirenone and have a 24-hour window instead of 3, making them a little more forgiving. But they’re still not as forgiving as combined pills. If you’re choosing between the two, consider your lifestyle. If you’re someone who wakes up at different times every day, a combined pill might be easier to manage.
What Are the Side Effects?
Side effects are why so many women stop taking the pill. But not all side effects are bad-and not all are permanent.
Most common side effects in the first few months include nausea, breast tenderness, spotting between periods, and mood swings. These usually fade after two to three cycles. If they don’t, it’s not necessarily a sign you’re allergic-it might mean you need a different formulation. Switching from levonorgestrel to drospirenone or norethindrone can make a big difference in how you feel.
Some women get headaches or migraines. If you develop new or worsening headaches, especially with visual changes or numbness, stop the pill and see a doctor. Estrogen can increase the risk of stroke in people with certain conditions, especially if you smoke, are over 35, or have high blood pressure.
Weight gain is often blamed on the pill, but large studies show the average weight gain is less than 2 pounds in the first year-and it’s often water retention, not fat. If you notice significant weight gain, look at your diet and activity level before blaming the pill.
On the flip side, many women experience real benefits. The pill can make periods lighter, more regular, and less painful. It reduces PMS symptoms for many. It can clear up acne, especially with pills containing drospirenone, which are FDA-approved for acne treatment. It also lowers the risk of ovarian, endometrial, and colon cancer. Women who take the pill for five years cut their ovarian cancer risk by almost a third. That protection lasts for decades after stopping.
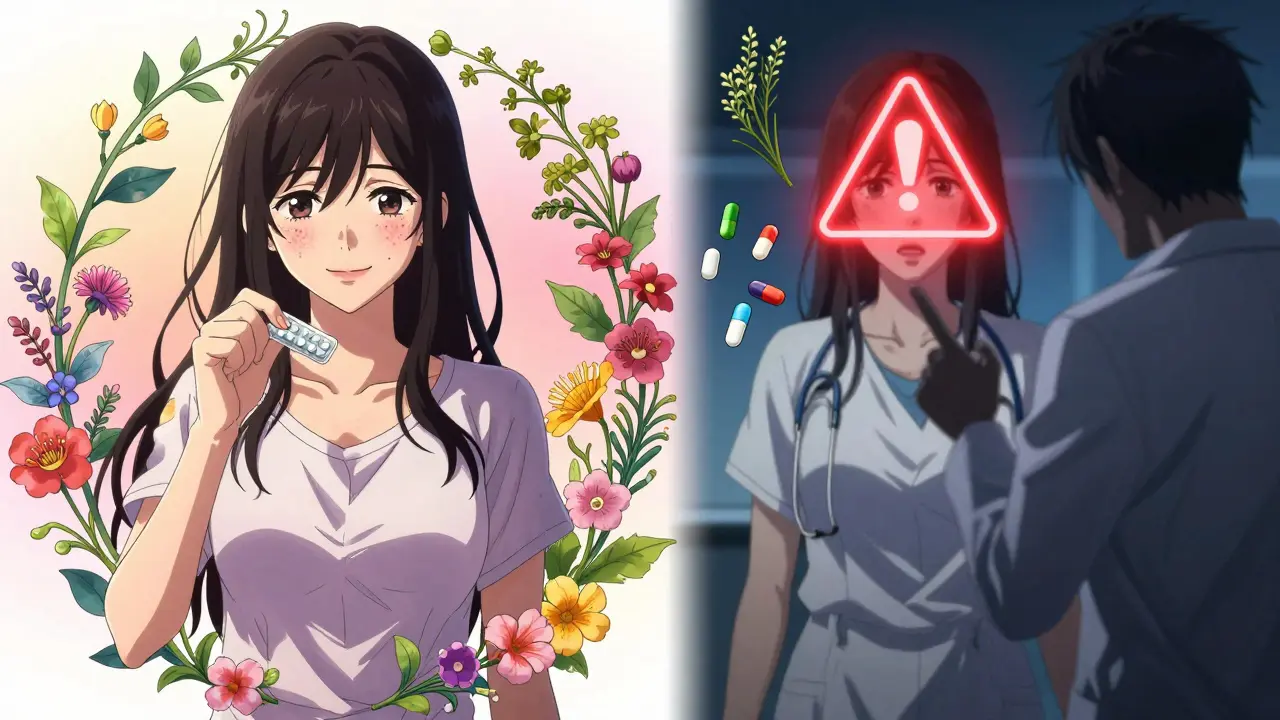
What Medications and Supplements Can Interfere?
This is where things get dangerous-and why so many women get pregnant unexpectedly.
Some antibiotics, like rifampin, can make the pill useless. But it’s not just antibiotics. Anti-seizure drugs, certain HIV medications, and even the herb St. John’s Wort can reduce hormone levels enough to cause ovulation. Even some antifungal pills and tuberculosis treatments interfere.
Here’s the scary part: most doctors don’t ask about supplements. If you’re taking St. John’s Wort for depression, turmeric for inflammation, or milk thistle for liver health, you’re at risk. These aren’t just ‘natural’-they’re active drugs that interact with your hormones.
Even some over-the-counter pain relievers like ibuprofen can slightly reduce the pill’s effectiveness if taken daily over long periods. That’s not common, but it’s documented. If you’re on long-term NSAIDs, talk to your doctor.
And don’t assume your pharmacist will catch it. Pharmacists are busy. You have to be your own advocate. Always ask: ‘Will this interfere with my birth control pill?’ before starting any new medication, supplement, or herbal remedy.
What About Long-Term Use?
Some women worry about taking the pill for years. Is it safe? Can you get pregnant after stopping?
Yes, you can. Most women get their period back within 90 days after stopping the pill. Fertility returns quickly. There’s no evidence that long-term use damages fertility. In fact, women who’ve used the pill for over five years often conceive faster than those who’ve never used it.
The biggest risk with long-term use is blood clots-but only if you have other risk factors. Smoking after age 35? High blood pressure? Obesity? Family history of clots? Then the pill isn’t for you. But if you’re healthy, under 35, and don’t smoke, the risk is extremely low. Modern pills with lower estrogen doses have made this safer than ever.
Some women stay on the pill for 10, 15, even 20 years. It’s fine. The key is regular check-ups. Your blood pressure should be checked yearly. If you develop new symptoms-like chest pain, leg swelling, or sudden vision changes-stop the pill and get help immediately.
When Should You Avoid Birth Control Pills?
There are clear medical reasons not to use hormonal birth control:
- History of blood clots, stroke, or heart attack
- Uncontrolled high blood pressure
- Severe liver disease
- Known or suspected breast cancer
- Migraines with aura (flashing lights, blind spots, numbness)
- Smoking and over age 35
- Undiagnosed abnormal vaginal bleeding
If any of these apply to you, talk to your doctor about alternatives. IUDs, implants, or progestin-only shots might be safer. The pill isn’t the only option-and it’s not always the best one.

What About STIs?
Birth control pills do nothing to protect against sexually transmitted infections. Not one bit. If you’re having sex with someone new-or even with someone you’ve been with for a while-condoms are still necessary. The pill protects against pregnancy. Only condoms protect against chlamydia, gonorrhea, HIV, and other infections.
Many women assume that if they’re on the pill, they don’t need condoms. That’s a dangerous myth. STIs can cause infertility, chronic pain, and long-term health problems-even if you never have symptoms.
Use condoms. Always. Especially if you’re not in a monogamous relationship. The pill gives you peace of mind about pregnancy. Condoms give you peace of mind about everything else.
How to Make the Pill Work for You
If you’re going to use the pill, make it work. Here’s how:
- Take it at the same time every day. Tie it to brushing your teeth or eating dinner.
- Set a daily phone alarm. Don’t rely on memory.
- If you miss a pill, take it as soon as you remember. If it’s more than 24 hours late (or 3 hours for mini-pills), use backup contraception for 7 days.
- Keep extra packs on hand. Travel with them. Keep one at work.
- Never skip the placebo week unless your doctor says to. Skipping can cause breakthrough bleeding and reduce effectiveness.
- Always tell your doctor about every medication and supplement you take-even if you think it’s harmless.
There’s no shame in needing help remembering. Apps like MyPill or Birth Control Reminder can send you daily alerts. Some pharmacies even offer blister packs with alarms built in.
The pill isn’t perfect. But for millions of women, it’s the right choice. It’s reversible. It’s private. It helps with acne and cramps. And if you use it correctly, it’s one of the most reliable ways to control your fertility.
Just don’t treat it like a casual habit. Treat it like the medicine it is.
Can I take birth control pills if I smoke?
If you’re over 35 and smoke, you should not take combined birth control pills. Smoking increases the risk of blood clots, heart attack, and stroke-especially when combined with estrogen. If you’re under 35 and smoke, talk to your doctor. You may still be able to use progestin-only pills, which don’t contain estrogen and carry much lower risk.
Do birth control pills cause weight gain?
Most studies show minimal weight gain-less than 2 pounds on average in the first year. Any increase is usually due to water retention, not fat. If you notice significant weight gain, consider diet, stress, or other medications. Switching pill types might help, but weight gain isn’t a guaranteed side effect.
How soon after stopping the pill can I get pregnant?
Fertility returns quickly. Most women have their first period within 90 days after stopping the pill. Many conceive within the first few months. There’s no evidence that long-term use delays fertility. You don’t need to wait before trying to get pregnant.
Can I skip my period by taking birth control pills continuously?
Yes. Many women skip the placebo week and start a new pack right away to avoid periods. This is safe for most people and can reduce cramps, headaches, and PMS. Talk to your doctor first, especially if you’ve never done it before. Breakthrough bleeding is common at first but usually improves over time.
What should I do if I miss two pills in a row?
Take both missed pills as soon as you remember-even if that means taking two pills in one day. Then continue with your regular schedule. Use condoms or avoid sex for the next 7 days. If you had unprotected sex in the past 5 days, consider emergency contraception. Missing two pills increases pregnancy risk significantly.
Are generic birth control pills as effective as brand-name ones?
Yes. The FDA requires generic pills to have the same active ingredients, strength, and absorption rate as brand-name versions. They’re just cheaper. Some women report differences in side effects, which may be due to inactive ingredients like fillers or dyes. If you have issues with a generic, ask your doctor about switching to another generic or the brand.
Next Steps: What to Do Now
If you’re thinking about starting the pill, make an appointment with your doctor or a sexual health clinic. Bring a list of everything you take-medications, supplements, even herbal teas. Ask about your personal risk factors. If you’ve had migraines, blood clots, or high blood pressure, be upfront.
If you’re already on the pill and you’ve missed doses, or you’re worried about interactions, don’t wait. Talk to your pharmacist or doctor. You might need to switch types or add backup protection.
And if you’re tired of remembering a daily pill, consider long-acting options like IUDs or implants. They’re more effective, require less effort, and cost less over time. The pill is great-but it’s not the only option. Choose what fits your life, not just what’s advertised.
Comments (15)
-
Eli In January 29, 2026I took the pill for 5 years and never missed one. My periods got lighter, my skin cleared up, and I didn't gain a pound. 🌸 It's not magic, but when you treat it like medicine, it works.
-
Kristie Horst January 30, 2026You say 'don't treat it like a casual habit'... yet the entire pharmaceutical industry markets it exactly that way. The irony is thick enough to spread on toast.
-
Kacey Yates February 1, 2026St johns wort is a big no no i cant believe doctors dont tell you this i had a friend get pregnant because she thought herbal meant safe lol
-
Sheryl Dhlamini February 3, 2026I switched from combined to mini-pill after my migraines got worse. The 3-hour window is brutal. I set 7 alarms. Still missed one once. Panic mode for a week. 😅
-
Doug Gray February 4, 2026The 93% efficacy rate is a statistical illusion rooted in neoliberal individualism. The system fails you by making reproductive autonomy contingent on perfect compliance. The pill isn't broken-it's a product of a flawed paradigm.
-
kabir das February 5, 2026I'm from India, and here, pharmacists sell birth control pills without prescription... no one asks about antibiotics or supplements... I'm terrified now...
-
Robin Keith February 6, 2026The real tragedy isn't the missed pill-it's the cultural expectation that women should be the sole arbiters of reproductive responsibility. Why isn't there a male pill? Why do we still treat contraception as a female burden? The patriarchy doesn't just enable this-it designs it.
-
Keith Oliver February 7, 2026Bro I took the pill for a year and my boobs got huge. Then I started taking turmeric and got pregnant. So yeah, supplements are wild. Also I think my ex was cheating. Just saying.
-
LOUIS YOUANES February 8, 2026I don't get why people are so obsessed with the pill. Just get an IUD. It's cheaper, better, and you don't have to think about it. Why are we still talking about this like it's 1998?
-
Andy Steenberge February 9, 2026I’ve worked in sexual health for 12 years. The biggest gap isn’t knowledge-it’s access. Women who work two jobs, don’t have insurance, or live in rural areas can’t afford to be perfect. The pill’s 93% efficacy is a luxury metric. We need better systemic support, not just better reminders.
-
Laura Arnal February 11, 2026I skipped my period for 18 months using the pill and it changed my life. No more cramps on weekends, no more panic-buying pads at 2am. 🙌 If your doctor says no, find one who gets it.
-
ryan Sifontes February 13, 2026They say birth control pills lower cancer risk but what about the ones that cause breast cancer? Nobody talks about that. And what if your mom had it? What if your aunt? What if the estrogen is slowly cooking your cells from the inside? I don't trust pharma
-
Laia Freeman February 13, 2026I use my pill app and it’s life changing!! I set it for 8pm and it vibrates like a little angel whispering ‘don’t be a dumbass’ 😘 and I haven’t missed one in 3 years. Also I got my period on time for the first time ever. Bless this technology
-
paul walker February 14, 2026I'm a guy but my girlfriend takes the pill and I learned all this so I could help her. Set alarms together. Keep extras in my bag. Talk to the pharmacist. It's not her job alone. We're in this.
-
rajaneesh s rajan February 16, 2026You know what's funny? We treat the pill like a goddamn rocket launch-perfect timing, no errors, zero margin. But we don't treat insulin that way. Or blood pressure meds. Why? Because it's a woman's body. And somehow, that makes it less important.
