Getting insulin dosing wrong isn’t just a mistake-it can land you in the emergency room. One extra unit, the wrong syringe, or a miscalculated correction factor can send blood sugar crashing too low. Hypoglycemia doesn’t wait for perfect conditions. It strikes when you’re driving, sleeping, or rushing through lunch. And the worst part? Many of these errors are avoidable-if you know what to look for.
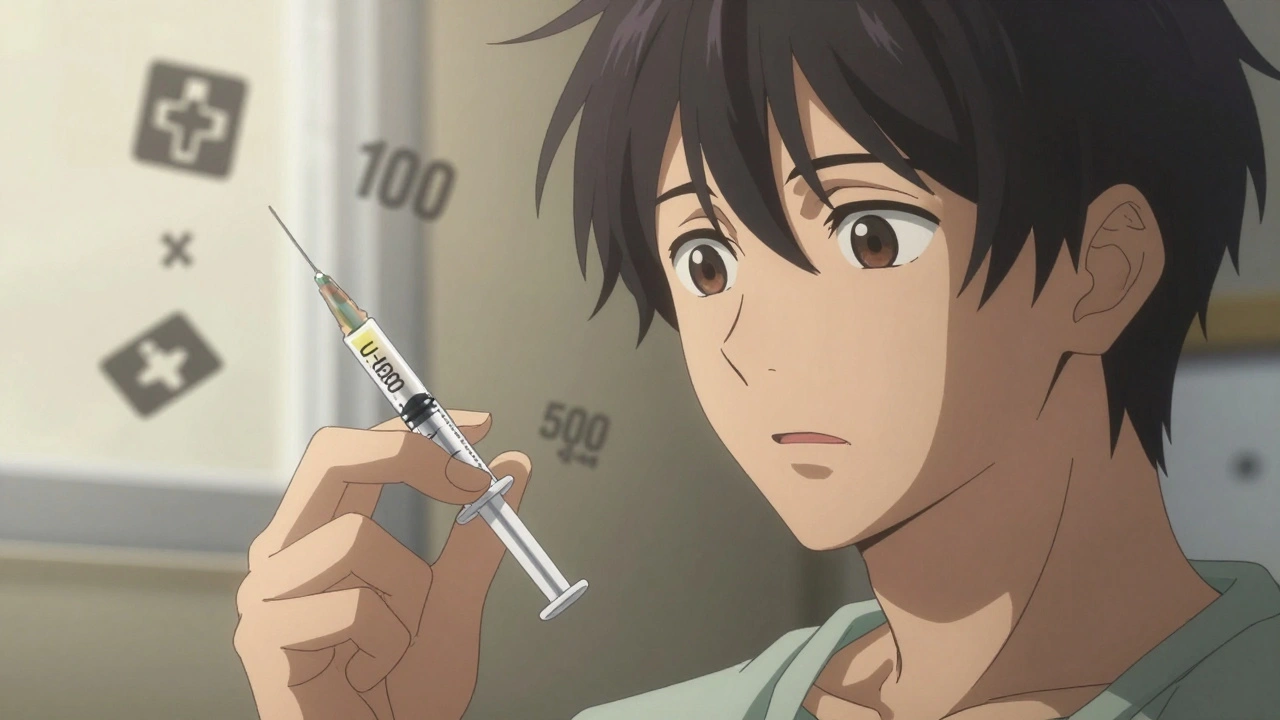
Understanding Insulin Concentrations: U-100 vs. U-500
Not all insulin is the same. The most common type you’ll see is U-100 insulin, which means 100 units per milliliter. That’s what most pens, syringes, and prescriptions are built for. But there’s also U-500 insulin, five times stronger. It’s used by people with severe insulin resistance, often those with long-standing Type 2 diabetes. Mixing them up is deadly. Using a U-100 syringe to draw U-500 insulin? You’ll give yourself five times the dose. That’s not a typo-it’s a life-threatening error.Always check the label. Not just once, but every single time. Look for the concentration: U-100 or U-500. If you’re switching brands or types, double-check with your pharmacist. Many hospitals now use color-coded labels and dedicated U-500 syringes to prevent this. At home, you don’t have that safety net. So be your own watchdog.
The Syringe That Could Save Your Life
Insulin syringes aren’t interchangeable with regular ones. They’re marked in units, not milliliters. A U-100 syringe holds up to 100 units, and each line equals 1 or 2 units depending on the size. If you use a 0.5 mL syringe (common for vaccines) to draw insulin, you’ll misread the volume entirely. You might think you’re giving 10 units, but you’re giving 50. Or worse-you think you’re giving 50, but you’re only giving 10.Always use a syringe designed for insulin. They come in three sizes: 0.3 mL (up to 30 units), 0.5 mL (up to 50 units), and 1.0 mL (up to 100 units). Pick the smallest one that fits your dose. Smaller syringes have bigger, clearer markings. That makes it easier to read. If you’re giving 12 units, a 0.3 mL syringe is safer than a 1.0 mL one. Less room for error.
And never reuse syringes. Even if you sterilize them. Reusing increases the risk of infection, blunted needles (which hurt more), and inaccurate dosing. The needle bends slightly after one use. That changes how much insulin flows through. It’s not worth the risk.
The Hidden Math: Why Your Correction Factor Might Be Wrong
You’ve probably heard of the “Rule of 1800.” It’s supposed to help you figure out how much one unit of rapid-acting insulin will drop your blood sugar. You take 1800, divide it by your total daily insulin dose, and that’s your correction factor. So if you take 40 units a day, 1800 ÷ 40 = 45. That means one unit lowers your blood sugar by about 45 mg/dL.But here’s the problem: many online calculators, apps, and even some doctor’s notes use the wrong number. They use 1500 instead of 1800. That’s not a typo-it’s a systemic error. A 2018 study in PubMed found that nearly 80% of published formulas and digital tools used the incorrect factor. If you’re using 1500, you’re overestimating how much insulin you need. You’ll give too much. And that leads to hypoglycemia.
Use 1800 for rapid-acting insulins like Humalog, NovoLog, or Fiasp. Use 1500 only if your doctor specifically tells you to-usually for people on very high doses or with unusual insulin sensitivity. Don’t guess. Ask your provider to confirm your correction factor. Write it down. Put it on your phone. Don’t rely on memory.

Carb Counting and the 500 Rule
You also need to know how much insulin covers your carbs. The “500 Rule” helps: 500 ÷ total daily insulin dose = grams of carbs covered by one unit. So if your total daily dose is 50 units, 500 ÷ 50 = 10. That means one unit covers 10 grams of carbs.But here’s the catch: that number varies wildly from person to person. Some people need one unit for every 4 grams of carbs. Others need one unit for 30 grams. Your body’s insulin sensitivity changes with stress, illness, hormones, even sleep. That’s why your doctor starts you with a general number-then adjusts it over time.
Track your meals and blood sugar. Did your sugar spike after eating 60 grams of carbs and taking 6 units? That’s 10 grams per unit. Did it drop too low? Maybe you need 12 grams per unit. Keep a log. Bring it to your next appointment. Don’t assume your initial number is permanent.
Switching Insulin Types? Don’t Guess
If you’re switching from NPH to Lantus, or from Tresiba to Basaglar, you can’t just copy the same dose. The body absorbs these insulins differently. NPH is cloudy, peaks at 4-6 hours, and lasts 12-18 hours. Lantus and Basaglar are clear, last 24 hours, and have no real peak. Tresiba lasts over 42 hours. They’re not interchangeable.When switching from NPH to Lantus, reduce your dose by 20%. If you were on 60 units of NPH, start with 48 units of Lantus. Going from Tresiba to Basaglar? If you were on 100 units of Tresiba once daily, split that into 40 units twice daily-80% of your original dose. These aren’t suggestions. They’re clinical guidelines backed by manufacturer data and the American Diabetes Association.
Always talk to your provider before switching. Don’t rely on a friend’s advice or an article you read online. Even small changes in timing or dose can trigger low blood sugar in the first few days.
How to Spot and Stop Hypoglycemia Before It’s Too Late
Hypoglycemia means your blood sugar is below 70 mg/dL. Symptoms? Shaking, sweating, dizziness, confusion, rapid heartbeat. But here’s the scary part: after years of diabetes, your body stops warning you. That’s called hypoglycemia unawareness. You feel fine-until you pass out.Prevention starts with checking your blood sugar. Not just before meals. Before bed. After exercise. When you feel “off.” If you’re on insulin, test at least 4 times a day. More if you’re adjusting doses.
Always carry fast-acting sugar. Glucose tabs. Juice. Hard candy. Don’t rely on candy bars or cookies-they have fat and protein that slow absorption. Glucose tabs work in 10-15 minutes. Take 15 grams, wait 15 minutes, check again. Repeat if needed. Then eat a snack with protein and carbs to keep your sugar stable.
If you’re alone and can’t treat yourself, wear a medical alert bracelet. Tell someone close to you how to give you a glucagon shot. Glucagon kits are easy to use now-no mixing required. Just inject. It’s life-saving.

Titration: How to Adjust Your Dose Safely
Basal insulin (like Lantus or Tresiba) is usually adjusted based on fasting blood sugar. Here’s a simple, safe approach:- If fasting sugar is < 60 mg/dL → reduce dose by 4+ units
- If fasting sugar is 60-99 mg/dL → reduce by 2 units
- If fasting sugar is 100-139 mg/dL → no change
- If fasting sugar is 140-159 mg/dL → increase by 2 units
- If fasting sugar is 160-179 mg/dL → increase by 4 units
- If fasting sugar is ≥ 180 mg/dL → increase by 6-8 units
Make changes slowly. Only adjust once every 3-5 days. Too many changes too fast = unstable blood sugar. And never adjust mealtime insulin without knowing your carb ratio and correction factor. One wrong move can cause a cascade of highs and lows.
Technology Can Help-But Don’t Rely on It Alone
Continuous glucose monitors (CGMs) are game-changers. They show trends, not just numbers. They alert you before you crash. But they’re not magic. You still need to understand how insulin works. A CGM won’t tell you if you’re using the wrong syringe. It won’t fix a math error. It won’t prevent you from confusing U-500 with U-100.Use tech as a tool, not a crutch. Pair your CGM with a logbook. Note your doses, meals, activity, and stress levels. Patterns emerge over time. That’s how you learn what your body really needs.
Final Rule: When in Doubt, Do Less
It’s better to be a little high than dangerously low. If you’re unsure about your dose, skip it-or take half. Eat a snack. Check your sugar in an hour. You can always add more later. But once you inject too much insulin, you can’t undo it. Hypoglycemia can kill in minutes. And recovery isn’t always guaranteed.Insulin saves lives. But it demands respect. Know your numbers. Know your syringes. Know your conversion factors. And never assume. Ask. Double-check. Write it down. Your life depends on it.
Comments (9)
-
Lucy Kavanagh December 6, 2025
So let me get this straight - the government and Big Pharma are secretly pushing U-500 insulin on people so they can charge more and keep us dependent? I’ve seen the docs - they’re all in on it. My cousin’s nurse said the syringes are color-coded to trick us into thinking we’re safe. But I checked the FDA’s leaked internal memo - it’s all about control. I’m switching to herbal tea and moonlight fasting now. 🌙🍵
-
Chris Brown December 8, 2025
It is, in fact, a matter of profound moral negligence that individuals are left to self-administer life-threatening medications without mandatory oversight. The notion that one can rely on personal vigilance - rather than institutional safeguards - is not merely irresponsible, it is an affront to the very principles of public health. One does not entrust nuclear codes to a child. Why, then, insulin?
-
Stephanie Fiero December 10, 2025
OMG YES THIS. I used a vaccine syringe once bc I was in a rush and nearly died. Like, literally thought I was gonna pass out in the grocery store. Don’t be me. Get the right syringe. The 0.3ml ones are like, so much easier to read. I keep mine in a labeled pouch with my glucagon. You’re not lazy if you double check - you’re smart. 💪
-
Laura Saye December 11, 2025
The existential weight of insulin dosing is not merely clinical - it is ontological. Each unit represents a choice between autonomy and annihilation. We navigate a world where our bodies are both temple and machine, and the margin between equilibrium and collapse is measured in decimal points. The 1800 rule isn’t just math - it’s a covenant with mortality. To misapply it is to misread the silence between heartbeats. I carry glucose tabs not for survival, but as a ritual of remembrance - that I am still here, because I chose to be careful.
-
Krishan Patel December 12, 2025
Let me correct the misinformation in this post. The 1800 rule is not universally applicable. It assumes a linear pharmacokinetic model, which is invalid for insulin resistance phenotypes. In South Asian populations, insulin sensitivity is significantly lower due to adipocyte distribution and genetic polymorphisms in the IRS-1 gene. Therefore, using 1500 is not an error - it is an empirical adaptation. You are not safer by blindly following Western guidelines. Your body is not a white American male. Stop conflating protocol with physiology.
-
Carole Nkosi December 14, 2025
Insulin is not medicine. It is a weapon of economic oppression. The pharmaceutical industry created this entire system - U-100, U-500, CGMs, the 500 rule - so you’d feel like you’re managing your health, when really you’re just feeding their profits. I’ve been on insulin for 18 years. I’ve never once trusted a label. I use my own calibrated dropper and calculate everything by moon phase. You think you’re safe? You’re just another statistic waiting to happen.
-
Jennifer Patrician December 14, 2025
Wait - so you’re telling me that the FDA doesn’t require insulin pens to have a built-in voice assistant that screams ‘THIS IS U-500’ when you pick it up? That’s insane. And why aren’t all syringes made with biometric fingerprint locks? I mean, if my phone can unlock with my face, why can’t my insulin? Someone’s got to sue these companies. This is a Class A negligence crisis.
-
Jimmy Jude December 15, 2025
Let me tell you about the night I nearly died because I used the wrong syringe. I was 22. I thought I knew what I was doing. I didn’t. I woke up in the ER with my mom screaming, ‘HE’S NOT BREATHING!’ They had to give me three vials of dextrose. I’ve never touched a syringe without double-checking since. And guess what? I’m still here. Not because I’m lucky. Because I listened. You think you’re too smart to make a mistake? You’re not. You’re just not dead yet.
-
Rupa DasGupta December 17, 2025
Ugh I just spent 3 hours crying because I misread my syringe and my sugar dropped to 42. I thought I was fine until I couldn’t stand up. Now I keep my glucose tabs in my bra and my phone on loud with a reminder that says ‘CHECK THE LABEL’ every morning. 😭😭😭 I’m not okay but I’m trying. And if you’re reading this - please, please, please don’t be like me. You’re worth more than one wrong unit.
