
Key Takeaways
- nimodipine is a calcium‑channel blocker that specifically targets the brain’s blood vessels.
- It improves outcomes after subarachnoid hemorrhage by reducing cerebral vasospasm.
- Emerging research suggests it may help with cognitive decline and certain forms of vertigo.
- Typical dosing is 60 mg every 4 hours for 21 days, but adjustments are needed for liver issues.
- Side‑effects are usually mild-headache, dizziness, or low blood pressure-yet they should be monitored.
What is Nimodipine?
When you hear the name nimodipine is a lipophilic dihydropyridine calcium‑channel blocker that preferentially dilates cerebral arteries. It was first approved in the early 1990s to treat complications from brain bleeds, and its chemistry lets it cross the blood‑brain barrier much better than other drugs in its class.
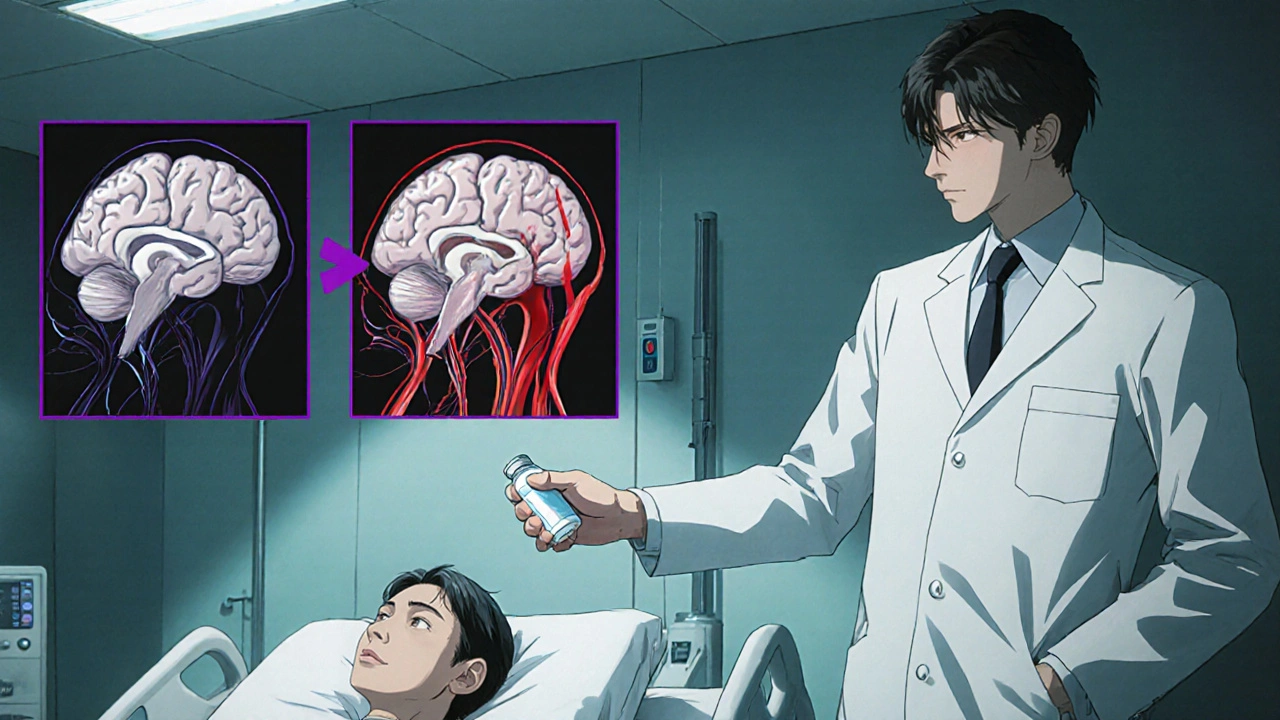
How Does Nimodipine Work?
At the cellular level, nimodipine blocks L‑type calcium channels (the “L‑type calcium channel” is a type of protein that lets calcium ions enter smooth‑muscle cells). By limiting calcium influx, the drug relaxes the smooth muscle in blood‑vessel walls. The result? Wider vessels and better blood flow, especially in the brain where tight control of pressure is critical.
Think of it like loosening a garden hose that’s been kinked. The water (blood) can finally flow freely, delivering oxygen and nutrients to the parts of the brain that need them most.
Why Is Nimodipine Important for Neurological Health?
Neurological health hinges on two things: adequate blood supply and protection from toxic cascades after injury. Nimodipine tackles both:
- Subarachnoid hemorrhage-a bleed between the brain and its outer membrane-often leads to a dangerous narrowing of cerebral arteries called cerebral vasospasm. Nimodipine reduces the incidence and severity of that spasm.
- By improving circulation, it may limit secondary brain injury, giving neurons a better chance to survive.
- Its ability to cross the blood‑brain barrier opens the door for direct neuroprotective effects, something many systemic drugs can’t achieve.
Clinical Evidence: Subarachnoid Hemorrhage
Large randomized trials from the 1990s (the International Cooperative Aneurysm Study) showed that patients who received nimodipine had a 30 % lower risk of death or severe disability compared with placebo. Follow‑up meta‑analyses in 2022 still confirm a relative risk reduction of about 0.7 for poor outcomes.
In practical terms, that means if 10 out of 100 patients would normally end up with major deficits after a bleed, nimodipine can bring that number down to 7.
Beyond Bleeds: Potential Uses in Cognitive Decline
Researchers have started looking at nimodipine for conditions where blood flow to the brain gradually worsens, such as vascular dementia and age‑related cognitive decline. A 2023 double‑blind study involving 120 older adults found that daily nimodipine improved scores on the Mini‑Mental State Examination (MMSE) by an average of 2.3 points after six months.
While these findings are promising, they’re still early‑stage. The drug isn’t yet approved for this purpose, but clinicians sometimes prescribe it off‑label when standard therapies fall short.
Vertigo and Migraine‑Associated Dizziness
Because nimodipine relaxes inner‑ear blood vessels, a handful of small trials have examined its role in treating refractory vertigo. One 2021 trial reported that 68 % of patients experienced a meaningful reduction in dizziness after a two‑week course.
If you’ve ever felt the world spin for no clear reason, this could be an alternative to traditional antihistamines or vestibular rehab-though you’d need a doctor’s green light.
Dosage, Administration, and Safety
Standard protocols for subarachnoid hemorrhage call for 60 mg taken orally every four hours for 21 days. For off‑label uses, doctors may prescribe 30 mg twice daily, but that varies.
Key safety points:
- Take the medication with food to reduce stomach irritation.
- Monitor blood pressure; nimodipine can cause hypotension, especially in the elderly.
- Liver function should be checked before starting, as the drug is metabolized hepatically.
- Avoid grapefruit juice-it interferes with the enzyme that clears nimodipine.
If you notice a sudden headache, fainting, or severe dizziness, contact your healthcare provider right away.
Comparing Nimodipine to Other Calcium‑Channel Blockers
| Attribute | Nimodipine | Nicardipine | Amlodipine |
|---|---|---|---|
| Primary Indication | Prevent cerebral vasospasm | Hypertensive emergencies | Chronic hypertension |
| Blood‑Brain Barrier Penetration | High | Low | Low |
| Typical Dose (adult) | 60 mg q4h (21 days) | 5‑10 mg/h IV | 5‑10 mg daily |
| Common Side‑effects | Dizziness, hypotension | Reflex tachycardia | Peripheral edema |
| Metabolism | Hepatic (CYP3A4) | Hepatic (CYP3A4) | Hepatic (CYP3A4) |
The table shows why nimodipine is the go‑to choice when brain‑specific vasodilation is needed. It’s not meant for routine blood‑pressure control.
Potential Pitfalls and How to Avoid Them
Even a well‑studied drug can trip you up if you ignore the details. Here are the most common mistakes:
- Skipping the loading phase. Some clinicians start with a lower dose to avoid sudden drops in blood pressure, but the evidence suggests the full 60 mg dose is needed to get the neuroprotective effect.
- Mixing with other vasodilators. Combining nimodipine with nitrates or other calcium‑channel blockers can push blood pressure too low.
- Ignoring liver health. Patients with moderate to severe hepatic impairment may need a 50 % dose reduction.
- Stopping abruptly. A sudden halt can cause rebound vasoconstriction. Taper over a few days if you need to discontinue.
Frequently Asked Questions
Can nimodipine improve memory in healthy adults?
Current research focuses on patients with brain injury or vascular risk. In healthy people, there’s no solid evidence that it boosts memory, and off‑label use isn’t recommended.
What should I do if I miss a dose?
Take the missed dose as soon as you remember unless it’s almost time for the next one. In that case, skip the missed dose-don’t double up.
Is nimodipine safe during pregnancy?
Animal studies have shown risk to the fetus, and human data are limited. It’s classified as Pregnancy Category C, so it should only be used if the potential benefit outweighs the risk.
How long does it take to see effects?
For subarachnoid hemorrhage, benefits start within the first 48 hours and continue throughout the 21‑day course. For cognitive studies, noticeable changes were reported after three to six months.
Can I take nimodipine with other blood pressure meds?
Yes, but only under a doctor’s supervision. Combining with other vasodilators can cause excessive hypotension, so dose adjustments are often needed.
Bottom Line: Should You Consider Nimodipine?
If you or a loved one have suffered a subarachnoid bleed, nimodipine is a cornerstone of care-nothing else matches its brain‑specific action. For other neurological concerns, the evidence is growing but still not definitive. Talk to a neurologist or a pharmacist who knows your medical history before starting, especially if you have liver disease or take multiple heart‑related drugs.
In short, the drug offers a unique blend of vascular support and possible neuroprotection, but like any medication, it works best when paired with proper monitoring and a clear treatment plan.
Comments (11)
-
Lennox Anoff October 24, 2025
The sanctity of cerebral perfusion is not a mere biochemical footnote but a moral imperative for any civilized society.
To ignore the proven merits of nimodipine in safeguarding the vulnerable brain after a hemorrhagic catastrophe is tantamount to willful neglect.
Its lipophilic grace, allowing it to traverse the blood‑brain barrier with unerring purpose, distinguishes it from the pedestrian calcium‑channel antagonists that crowd the pharmacy shelves.
When a patient confronts the specter of vasospasm, the drug acts as a vigilant custodian, easing the arterial constriction that would otherwise enslave neural tissue.
The historical trials of the International Cooperative Aneurysm Study have etched into the annals of medicine an unequivocal reduction in mortality and severe disability.
Such evidence should not be dismissed with the casual flippancy of a fad‑seeking enthusiast.
Moreover, the emerging data on cognitive decline, though nascent, hint at a future where nimodipine might stall the inexorable march of vascular dementia.
This prospect obliges us, as custodians of public health, to fund rigorous investigations rather than consign the drug to the shadows of obscurity.
The pharmacokinetic profile, reliant on hepatic metabolism via CYP3A4, demands respect for hepatic function and vigilance against grapefruit‑induced toxicity.
Physicians who cavalierly prescribe it without adjusting for liver impairment risk transforming a neuroprotective ally into a harbinger of hypotension.
The dosing regimen of sixty milligrams every four hours, though arduous, is justified by the narrow therapeutic window within which the brain thrives.
Any deviation, be it a careless dose reduction or an abrupt cessation, invites rebound vasoconstriction that can undo the hard‑won gains of therapy.
Let us also acknowledge that nimodipine is not a panacea for hypertensive maladies; its utility is confined to the cerebral microcosm, and misapplication elsewhere betrays a lack of scientific rigor.
The ethical physician must therefore wield this medication with precision, informed consent, and an unwavering commitment to monitoring.
In sum, to champion nimodipine is to champion a principle: that we owe our patients the most targeted, evidence‑based interventions available.
To waver in this duty is to abandon the very ethos of compassionate medicine.
-
Bianca Larasati October 27, 2025
Hey folks, this guide really shines a light on a drug that many of us only hear about in the ICU.
Think of nimodipine as the behind‑the‑scenes crew that keeps the brain’s plumbing clear when disaster strikes.
If you or someone you love is navigating a subarachnoid bleed, pushing for this medication can be a game‑changer.
Stay proactive, ask your neurologist about the dosing schedule, and don’t shy away from monitoring your blood pressure closely.
-
Lisa Woodcock October 31, 2025
Understanding how nimodipine works helps demystify the treatment pathway for patients and families alike.
Its ability to cross the blood‑brain barrier is a reminder that not all drugs are created equal.
When discussing options, consider the balance between potential benefits and the need for careful blood pressure monitoring.
Sharing this knowledge can empower loved ones to make informed decisions during a stressful time.
-
Zaria Williams November 3, 2025
Honestly, if you think you can just pop a pill and expect miracles, you’re missing the point.
People skip the liver check and end up dizzy as heck – that’s why doctors stress the monitoring.
Also, don’t even think about mixing it with grapefruit juice, that’s a rookie mistake.
Bottom line: follow the protocol or you’ll just waste money and risk your health.
-
ram kumar November 6, 2025
So we’re supposed to believe a cheap calcium blocker can rescue brains? Great story, but the reality is a bit more boring.
Unless you’re in a perfect clinical trial, the side‑effects can creep up and ruin the day.
Bottom line – use it only if you’re really desperate, and keep an eye on that blood pressure.
-
Melanie Vargas November 9, 2025
Let’s make sure everyone feels included in this conversation 😊.
If you’re starting nimodipine, set a reminder to take it with food – it helps with stomach irritation.
Don’t forget to check your BP daily; a quick log can show trends and keep your doctor in the loop.
We’ve got each other’s backs – stay safe and keep sharing tips! 👍
-
Charlie Stillwell November 12, 2025
While the enthusiasm is commendable, let’s inject some epistemic rigor here.
The pharmacodynamics of nimodipine demand a nuanced appraisal beyond anecdotal optimism.
One must consider the CYP3A4 interaction matrix, especially in polypharmacy scenarios, to avert iatrogenic hypotension.
Furthermore, the off‑label cognitive trials suffer from limited sample sizes, rendering statistical power questionable.
Thus, clinicians should calibrate expectations and rely on robust biomarkers when extending use beyond hemorrhagic contexts. 🚀
-
Ken Dany Poquiz Bocanegra November 15, 2025
Nimodipine’s brain‑specific action makes it a unique tool in neurology.
-
krishna chegireddy November 18, 2025
Everyone’s talking about the “official” studies, but they never mention the hidden funding streams that dictate the narrative.
What if the drug’s popularity is a manufactured hype to keep the pharmaceutical giants happy?
We’re told to monitor blood pressure, yet the real agenda is to lock patients into long‑term monitoring programs.
Think about it: a simple calcium blocker becomes a gateway for endless follow‑ups and data collection.
Stay skeptical and demand transparency before you swallow another tablet.
-
Tamara Schäfer November 21, 2025
When we examine the mechanistic pathways of nimodipine, we see a graceful interplay between ion channel modulation and vascular dynamics.
It’s fascinating how a single molecule can influence both macro‑circulatory pressure and micro‑environmental oxygen delivery.
Patients with subarachnoid hemorrhage benefit from this dual action, yet the literature still debates the optimal duration of therapy.
Beyond that, preliminary data on cognitive preservation hint at a broader neuroprotective role, though the evidence remains nascent.
Clinicians must weigh these potentials against contraindications such as hepatic insufficiency.
In practice, a patient‑centered approach, with vigilant monitoring, remains the gold standard.
-
Buddy Bryan November 24, 2025
Listen, the data on nimodipine isn’t a free‑for‑all; you need to follow the dosing schedule precisely.
If you miss a dose, take it as soon as you remember unless the next dose is due – then skip it, no double‑ups.
Watch out for hypotension; a quick BP check before each dose can prevent nasty drops.
And whatever you do, keep your liver function panels up to date – the drug is metabolized there, and you don’t want a silent failure.
