When you hear the word vitiligo, you might think of white patches on the skin. But what most people don’t realize is that treating it isn’t about covering up those patches-it’s about restoring balance. Vitiligo isn’t just a cosmetic issue. It’s an autoimmune condition where the body attacks its own melanocytes, the cells that give skin its color. The result? Patches of skin lose pigment, sometimes spreading over time. For many, it’s not just about appearance-it’s about confidence, daily life, and even mental health.
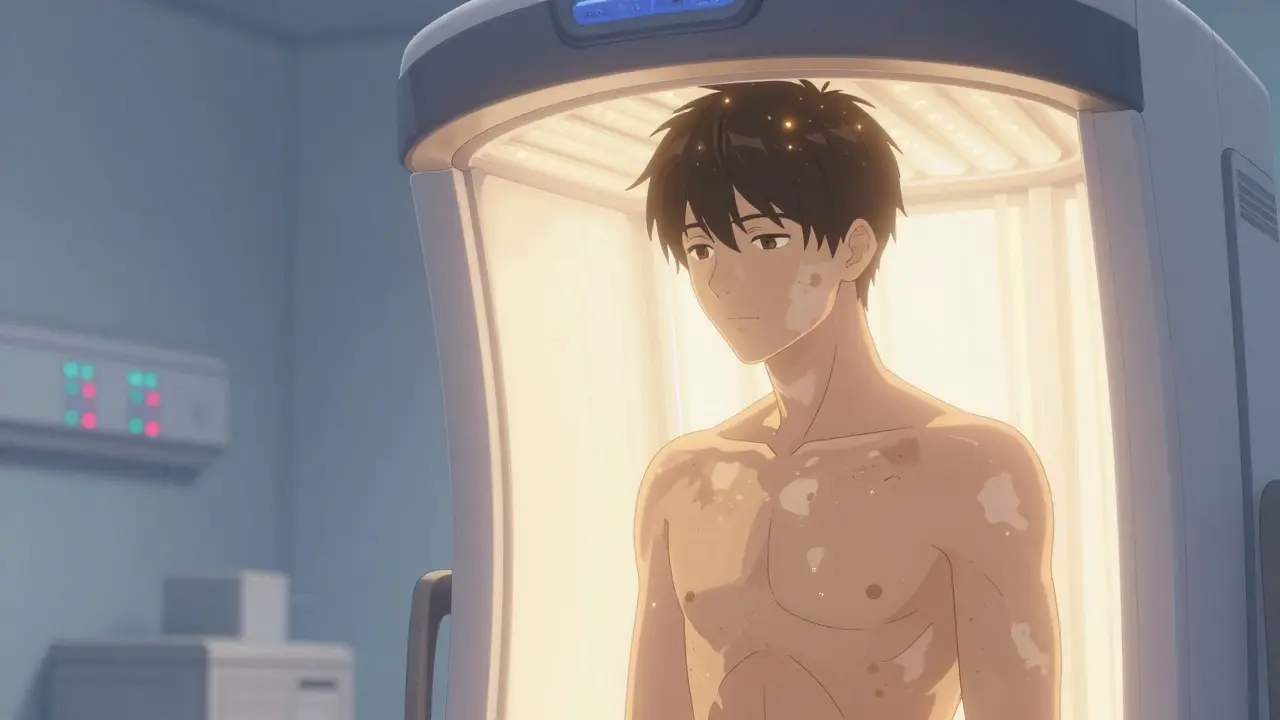
Phototherapy Isn’t What You Think
Many assume phototherapy means tanning beds or sunbathing. It doesn’t. Medical phototherapy for vitiligo uses controlled, targeted ultraviolet light to stimulate the remaining melanocytes hidden in hair follicles. The goal? Repigmentation-not darkening healthy skin, but bringing color back to the white patches. The most common and effective form today is narrowband ultraviolet B (NB-UVB), with a wavelength of 311-313 nm. It’s safer than older methods like PUVA, which used psoralen drugs and UVA light. PUVA carries higher risks: nausea in up to 30% of patients and a 13-fold increase in squamous cell carcinoma after 200+ treatments. NB-UVB? No drugs. No systemic side effects. Just light. Studies show that after six months of twice-weekly NB-UVB sessions, about 37% of patients see at least half their patches repigment. By 12 months, that number jumps to over 56%. For facial skin-where melanocytes are more active-response rates hit 70-80%. But hands and feet? Only 15-20% repigmentation even after a full year. That’s why treatment plans are personalized. You can’t expect the same results everywhere.Depigmentation Is a Different Path
Here’s where confusion often starts. The phrase “depigmentation and phototherapy combination” sounds like they’re used together. They’re not. Depigmentation is a completely separate strategy-and only for extreme cases. When more than 80% of your skin is affected, doctors may suggest depigmentation. This means using a topical cream called monobenzone to lighten the remaining pigmented areas until they match the white patches. It’s permanent. It’s irreversible. And it’s only considered when repigmentation efforts have failed or aren’t realistic. This isn’t a shortcut. It’s a last-resort decision. Patients need to understand the psychological impact. You’re not treating the disease-you’re adapting to it. Most people don’t choose this unless they’ve tried everything else. And no, you don’t combine it with phototherapy. That would be like trying to paint a wall white while also trying to repaint it red. The goals oppose each other.Why NB-UVB Is the Gold Standard
Since the late 1990s, NB-UVB has replaced PUVA as the go-to treatment. Why? Better safety, better results, and easier use. A 2017 JAMA Dermatology review of over 2,000 patients found NB-UVB led to 15-20% higher repigmentation than PUVA after a year. It’s now recommended by the American Academy of Dermatology, Mayo Clinic, NYU Langone, and UC Davis Health as first-line therapy for generalized vitiligo affecting more than 5% of the body. Treatment starts with a test to find your minimal erythema dose (MED)-the lowest UV dose that causes slight redness. This ensures you’re not under- or over-treated. Sessions begin at 2-3 times per week, each lasting seconds to minutes. Dose increases by 10-20% weekly, based on skin response. You need at least six months to judge if it’s working. Many give up before then.
Home vs. Clinic: What Works Better?
Going to a clinic twice a week for a year sounds exhausting. Travel, time off work, childcare-it adds up. That’s why home phototherapy units have become popular. Philips TL-01 and similar devices cost $2,500-$5,000 upfront, but Medicare covers 80% for qualifying patients since 2021. A 2020 study found home users were 35% more likely to stick with treatment than clinic patients. Why? No commute. No waiting room. More control. But there’s a catch: 22% more reported burns due to incorrect dosing. That’s why proper training matters. Apps that track sessions and doses improve adherence by 92%, according to UC Davis Health. If you go the home route, don’t skip the consultation. Don’t guess the settings.Combining Phototherapy With Topical Treatments
Here’s the real game-changer: phototherapy doesn’t work alone. It works better when paired with topical creams. Calcineurin inhibitors like tacrolimus or pimecrolimus-often used for eczema-are now routinely combined with NB-UVB. Mayo Clinic data shows this combo boosts repigmentation by 25-30%. Why? These creams calm the immune system locally, making it easier for melanocytes to recover. Even newer is ruxolitinib cream (Opzelura), an FDA-approved JAK inhibitor. A 2023 trial called Ruxotmel showed that when paired with NB-UVB, 54% of patients achieved over 50% repigmentation in just 24 weeks. That’s faster than phototherapy alone. This combo could cut treatment time by months.What About the Hands and Feet?
If your vitiligo is on your fingers, toes, or lips, you’re in the toughest group. These areas have fewer hair follicles, which means fewer melanocyte reservoirs. Even with perfect treatment, repigmentation is slow-or sometimes nonexistent. A Mayo Clinic survey found 89% of patients with hand vitiligo quit phototherapy by month 8 because they saw little change. That’s heartbreaking. But quitting doesn’t mean failure. It means it’s time to pivot. Options include camouflage makeup, micropigmentation (tattooing pigment into skin), or even accepting the condition with support.Cost, Time, and Real-Life Challenges
Phototherapy is affordable compared to newer drugs. A year of NB-UVB costs $1,200-$2,500. Ruxolitinib cream? Over $5,000 annually. But insurance doesn’t always cover it fully. In 2022, 43% of insured patients still paid over $1,000 out of pocket due to session limits. Time is the real barrier. 100-150 sessions per year. Two to three times a week. That’s like a part-time job. Many patients start strong, then fade out. Support groups like Vitiligo Support International (with 15,000+ members) help. So do apps that send reminders and log progress.What’s Next?
Research is moving fast. The VITCURE-2 trial, launching in early 2024, is testing afamelanotide implants-tiny rods that release a pigment-stimulating hormone-alongside NB-UVB. Early results suggest faster repigmentation. And then there’s AI. The Vitilux AI device, cleared by the FDA in October 2023, uses your smartphone camera to analyze patch size and skin tone, then auto-calculates your exact UV dose. In trials, it cut dosing errors by 37%. Imagine getting the right light every time, without guesswork.What Should You Do?
If you have vitiligo affecting less than 80% of your skin, phototherapy with NB-UVB is your best starting point. Add a topical cream like tacrolimus or ruxolitinib. Stick with it for at least six months. Track your progress with photos. Don’t compare your hands to your face-different areas respond differently. If your vitiligo is widespread and you’ve tried everything? Talk to your dermatologist about depigmentation. But understand: this isn’t treatment. It’s adaptation. And if you’re overwhelmed? You’re not alone. Thousands of people are walking this path. The goal isn’t perfection. It’s progress. One patch at a time.Can phototherapy and depigmentation be used together for vitiligo?
No, they cannot and should not be used together. Phototherapy aims to restore pigment to white patches, while depigmentation removes pigment from remaining colored skin to create a uniform appearance. These are opposite goals. Depigmentation is only considered when over 80% of the skin is affected and repigmentation treatments have failed or aren’t feasible.
How long does it take to see results from phototherapy for vitiligo?
Most people need at least six months of consistent treatment-typically two to three sessions per week-to see noticeable repigmentation. The 2017 JAMA Dermatology meta-analysis confirmed that three months is too short to judge effectiveness. Full results often take 12 to 18 months, especially for areas like the hands and feet.
Is NB-UVB safer than PUVA for vitiligo treatment?
Yes, NB-UVB is significantly safer. PUVA requires taking psoralen pills or applying it to the skin before UVA exposure, which increases risks like nausea, sunburn, and long-term skin cancer. Studies show PUVA carries a 13-fold higher risk of squamous cell carcinoma after 200+ treatments. NB-UVB doesn’t use chemicals, has fewer side effects, and has no proven link to melanoma even after 15 years of use.
Why does phototherapy work better on the face than the hands?
The face and neck have a higher density of melanocyte stem cells in hair follicles, which are the source of repigmentation. Hands and feet have far fewer follicles, so fewer cells are available to repopulate the white patches. Even with perfect treatment, repigmentation rates on hands and feet rarely exceed 20% after a full year.
Can I use a home phototherapy unit safely?
Yes, but only with proper training and adherence to protocol. Home units are just as effective as clinic-based treatment when used correctly. However, 22% more users report burns due to incorrect dosing. Use apps to track sessions, follow your dermatologist’s dose schedule exactly, and never increase exposure without professional guidance. Medicare and some insurers cover up to 80% of the cost for qualifying patients.
Are there new treatments that reduce the need for long-term phototherapy?
Yes. Combining NB-UVB with topical ruxolitinib cream (Opzelura) has shown promising results, with 54% of patients achieving over 50% repigmentation in just 24 weeks-faster than phototherapy alone. Emerging treatments like afamelanotide implants and AI-guided devices (like Vitilux AI) are also being tested to shorten treatment time and improve accuracy.
Comments (15)
-
swati Thounaojam January 8, 2026
Been using NB-UVB for 8 months-my face looks normal but my hands? Still white. Felt like giving up till I found that camouflage cream. Not magic, but it helps me leave the house.
Thanks for the post.
-
Ken Porter January 10, 2026
Why are we even talking about this? In America, we’ve got real health problems-obesity, diabetes, opioid crisis. Vitiligo? It’s a cosmetic issue wrapped in feel-good marketing. Stop making it a disease.
-
Molly Silvernale January 11, 2026
Phototherapy isn’t just light-it’s a quiet rebellion against the idea that skin must be uniform to be beautiful.
Every patch that returns is a whisper: ‘I am still here, still me.’
And yet… we’re told to ‘fix’ it, not to honor it.
Depigmentation? That’s not treatment-it’s surrender wrapped in a prescription.
But surrender, sometimes, is the bravest act of all.
Because who decides what ‘normal’ looks like? Not the skin. Not the light. Not the doctor.
It’s the person staring back in the mirror.
And maybe… just maybe… that’s the only cure that matters.
-
Joanna Brancewicz January 11, 2026
Topical JAK inhibitors like ruxolitinib are now first-line adjuncts in clinical practice due to their targeted immunomodulatory effects on the melanocyte microenvironment.
Combined with NB-UVB, they significantly reduce the time to repigmentation by inhibiting IFN-γ signaling pathways.
Adherence remains a challenge, but patient-reported outcomes show marked improvement in QoL metrics.
-
Evan Smith January 12, 2026
So… you’re telling me I can buy a $5,000 light box, burn my skin, and hope for color back? Sounds like a cult. But hey, if Medicare pays for it, I guess it’s legit.
Still, why not just get a tattoo? Faster, cheaper, and you pick the shade.
-
Dave Old-Wolf January 13, 2026
I started phototherapy after my daughter got diagnosed. We did it together-me in the chair, her on the other side with her little goggles. Six months in, her cheeks are slowly coming back. Not perfect. Not fast. But it’s something.
And honestly? Seeing her smile again… that’s worth every minute.
-
Prakash Sharma January 15, 2026
India has been using sunlight therapy for centuries-Ayurveda called it ‘Surya Chikitsa.’ Now Western medicine steals it, names it NB-UVB, and sells it for thousands. Why not just go outside? Free, natural, and no machine needed.
Stop overcomplicating everything.
-
Donny Airlangga January 16, 2026
That bit about hands and feet being harder to treat? I feel that. I’ve had vitiligo since I was 12. My fingers are still white. But I don’t hate them anymore. They’re mine. And that’s enough.
-
Kristina Felixita January 16, 2026
OMG I just got my home unit!! I’ve been using the Vitilux app to track sessions-game changer!!
Also, I made a playlist for my sessions: chill lofi + candles + tea. It’s my little ritual now.
And yes, I did burn my ankle once. Oops. But I learned!!
Don’t be scared-just be careful!!
-
Lois Li January 18, 2026
I used to think vitiligo was just a skin thing until I met someone who lost their job because coworkers said they looked 'sick.'
It’s not about pigment.
It’s about being seen as human.
And phototherapy? It’s not just healing skin-it’s helping people feel like they belong again.
That’s worth every session.
-
christy lianto January 18, 2026
My dermatologist said I’d need 150 sessions. I did 148 before I quit.
Not because I gave up.
Because I realized I didn’t need to be fixed.
My skin isn’t broken.
It’s just different.
And that’s okay.
-
Annette Robinson January 19, 2026
Thank you for writing this with such clarity and compassion.
It’s rare to see medical information that doesn’t feel cold or clinical.
People with vitiligo deserve to be heard-not just treated.
And you did that.
-
Luke Crump January 21, 2026
Wait-so we’re spending billions on light therapy because we can’t accept that skin doesn’t have to be one color?
What if the real problem isn’t vitiligo… but society’s obsession with uniformity?
What if the cure isn’t in the lamp… but in our minds?
And what if the doctors are just selling us a product to avoid facing that?
-
Manish Kumar January 22, 2026
Let me tell you something about vitiligo in India-my uncle had it, and they used turmeric paste, neem leaves, and sunlight every morning for years. No machines. No pills. Just tradition. And guess what? His patches faded slowly, naturally. Now, everyone wants to pay $5,000 for a machine that does the same thing? That’s capitalism, not medicine. We’ve forgotten that the body heals itself when given space, time, and respect. Modern medicine thinks it can outsmart nature. But nature doesn’t rush. It waits. And so should we.
-
Aubrey Mallory January 22, 2026
My sister tried ruxolitinib + phototherapy. After 16 weeks, her neck was 80% repigmented. But the cream cost $1,200 a month. Insurance denied it twice. We had to sell her laptop to pay for it.
So yes-it works.
But who gets to use it?
That’s the real question.
