
Autoimmune hepatitis isn’t caused by alcohol, viruses, or fatty foods. It’s when your own immune system turns on your liver-like a friendly fire incident inside your body. Instead of fighting off germs, your immune cells start attacking healthy liver tissue. The result? Chronic inflammation, scarring, and if left unchecked, liver failure. It’s rare-about 1 in 50,000 people have it-but it doesn’t care who you are. It hits women more often, shows up in teens and middle-aged adults, and sometimes sneaks in without symptoms until your blood test comes back wrong.
Two Types, One Problem
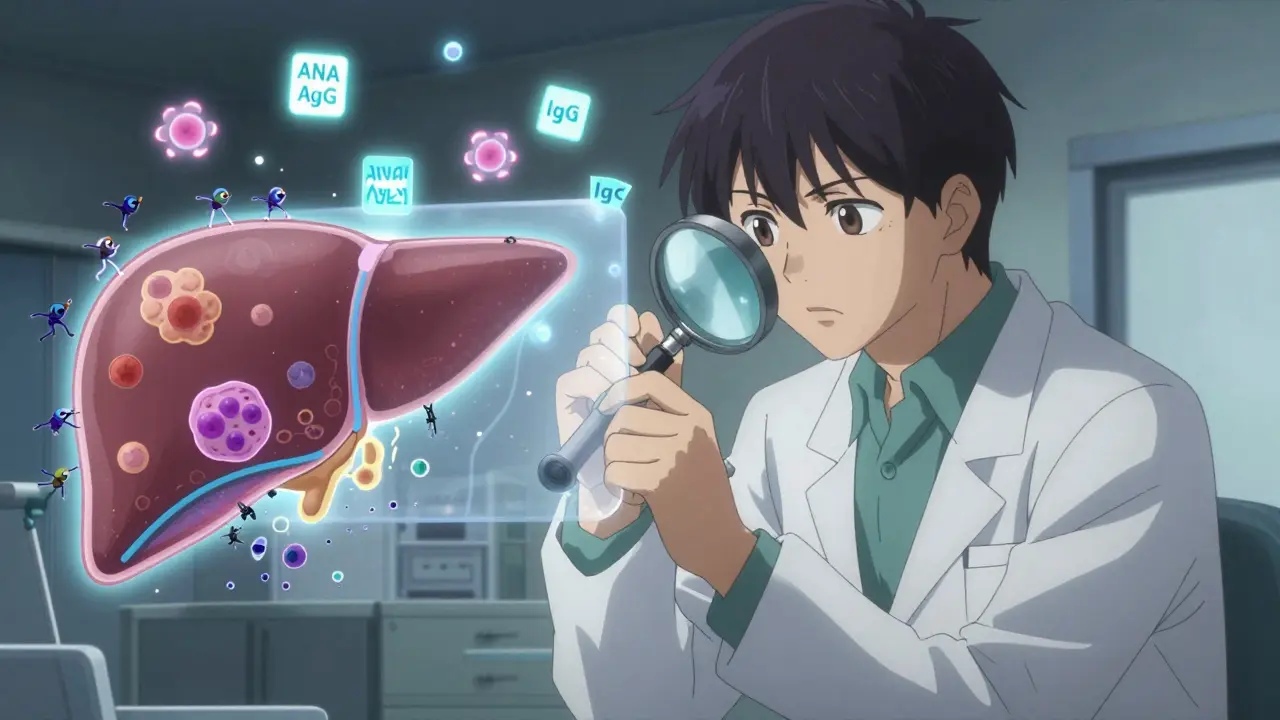
There are two main kinds of autoimmune hepatitis. Type 1 is the most common, making up 80 to 90% of cases in the U.S. and Europe. It usually shows up between ages 15 and 40, and it’s linked to antibodies called ANA and ASMA. These show up in blood tests and help doctors confirm the diagnosis. Type 2 is rarer and mostly affects children between 2 and 14 years old. It’s tied to different antibodies-LKM-1 and LC-1-that target liver proteins. Even though the types differ, the damage is the same: your liver gets inflamed, liver cells die, and over time, scar tissue builds up.
What makes it tricky is that the symptoms don’t always scream "liver disease." Some people feel fine until they collapse from fatigue. Others have joint pain, nausea, or dark urine. About 25% of patients come in with sudden symptoms that look just like hepatitis A or B-fever, yellow skin, vomiting. But here’s the difference: no virus is found. That’s why doctors don’t just test for viruses. They look for signs your immune system is misfiring.
How Doctors Diagnose It
There’s no single test for autoimmune hepatitis. It’s a puzzle. Doctors piece it together using blood work, imaging, and sometimes a liver biopsy. Blood tests usually show sky-high liver enzymes-ALT and AST-often five to ten times above normal. IgG levels, a type of antibody, are also elevated. That’s a red flag. If your IgG is more than 1.5 times the upper limit of normal and you don’t have hepatitis B or C, autoimmune hepatitis becomes the top guess.
The Revised International Autoimmune Hepatitis Group Scoring System, updated in 2022, helps doctors rate the likelihood. It adds up points for antibodies, IgG levels, liver histology, and the absence of viral causes. When used by experienced hepatologists, it’s 97% accurate. A liver biopsy isn’t always required, but it’s the gold standard. Under the microscope, you’ll see interface hepatitis-where immune cells eat away at the edge of liver lobules-and lymphoplasmacytic infiltrates, which look like crowds of immune cells camping out in the liver tissue.
One big pitfall? Mistaking it for drug-induced liver injury. About 1 in 5 people with autoimmune hepatitis are first told they reacted badly to a medication-maybe an antibiotic, a supplement, or even an over-the-counter painkiller. But if the symptoms keep getting worse after stopping the drug, and antibodies show up, it’s likely AIH. That’s why doctors don’t rush to blame medications. They wait, test, and retest.
What Happens If It’s Left Untreated
Without treatment, autoimmune hepatitis is deadly. Studies show that 90% of untreated patients die within 10 years. The liver doesn’t just get inflamed-it starts to scar. Fibrosis creeps in. Eventually, it turns to cirrhosis. Once cirrhosis sets in, complications follow: fluid in the belly, bleeding from swollen veins in the esophagus, confusion from toxins building up in the blood. The liver stops working. At that point, a transplant is the only option.
But here’s the good news: with treatment, survival rates jump to 94%. That’s not a guess. It’s from long-term data tracked across thousands of patients over decades. The difference between treatment and no treatment isn’t just about living longer-it’s about living without constant fatigue, without pain, without the fear of sudden collapse.
Standard Treatment: Steroids and Immunosuppressants
The go-to treatment has barely changed in 50 years-and it still works. It starts with prednisone, a corticosteroid that shuts down the immune system’s attack. Doctors usually begin with 0.5 to 1 mg per kilogram of body weight daily, capped at 60 mg. It’s a high dose at first, meant to get inflammation under control fast. But steroids come with a price: weight gain, insomnia, mood swings, bone thinning, and higher infection risk.
To reduce side effects, doctors add azathioprine. This drug helps keep the immune system suppressed without needing as much steroid. Most patients get both together. Within 3 to 6 months, liver enzymes start to drop. Complete remission-normal enzyme levels and IgG for at least two years-is achieved in 60 to 80% of people. That’s not a cure. It’s control. You’re not done taking meds. You’re just in a quieter phase.
Some people can’t tolerate azathioprine. Maybe they get nauseous, or their white blood cell count crashes. For them, mycophenolate mofetil is the next step. Studies show it works in 70 to 80% of those cases. It’s not FDA-approved for AIH, but it’s widely used because it’s effective and has fewer side effects than steroids alone.
Life on Immunosuppressants
Living with autoimmune hepatitis means living with medication-and its consequences. On patient forums, 82% of those on prednisone say they gained weight. Two-thirds report trouble sleeping. More than half deal with anxiety or depression. Fatigue is the most common complaint, reported by 78% of patients. It’s not laziness. It’s the inflammation still lingering, even when labs look good.
And then there’s the constant vigilance. You can’t skip blood tests. You need them every 2 to 4 weeks during the first few months. Then every 3 months once you’re stable. Why? To catch relapses early. If your ALT starts creeping up again, it means the disease is waking up. Catch it early, and you can adjust your meds before the liver gets damaged again.
You also need to protect your bones. Steroids weaken them. Doctors recommend calcium and vitamin D supplements daily. Some patients get bone density scans. You’re also more prone to infections. No live vaccines. No big crowds during flu season. Wash your hands. Tell every doctor you see you’re on immunosuppressants-even the dentist.

When Medications Don’t Work
About 10% of patients don’t respond to standard therapy. Their enzymes stay high. Their symptoms don’t improve. Their liver keeps scarring. These are the treatment-refractory cases. For them, options are limited. Some try newer drugs in trials-rituximab, which targets immune cells, or vedolizumab, which blocks inflammation in the gut and liver. Others get obeticholic acid, which the European Medicines Agency approved for AIH in 2022 based on early trial results showing nearly half of patients reached remission.
If all else fails, a liver transplant is the last resort. Autoimmune hepatitis is the fourth most common reason for adult liver transplants in the U.S., making up 6.2% of all cases. The good news? After transplant, the disease rarely comes back. The bad news? You’ll be on anti-rejection drugs for life, just like before. But now, you’re free from the worst of the fatigue and pain.
The Future of Treatment
Scientists are getting closer to personalized treatment. Research shows that people with certain gene variants-HLA-DRB1*03:01 and *04:01-are more likely to get autoimmune hepatitis and respond better to certain drugs. In the next 5 to 7 years, doctors may test for these genes before prescribing. That could mean less trial and error, fewer side effects, and higher remission rates.
New biomarkers are helping too. Anti-SLA/LP antibodies, once rare, are now used in diagnosis. When they show up, they boost diagnostic accuracy to 99%. That means fewer misdiagnoses and faster starts to treatment.
The global market for AIH drugs is growing fast-projected to hit $2 billion by 2028. But the real win won’t be in profits. It’ll be in patients who can live without constant fatigue, without fear, without being tied to a pill schedule that feels like a prison.
What You Can Do
If you’ve been diagnosed:
- Take your meds exactly as prescribed. Skipping doses is the #1 reason relapses happen.
- Get blood tests on schedule. Don’t wait until you feel bad.
- Ask for bone health support-calcium, vitamin D, maybe a DEXA scan.
- Report mood changes or infections right away.
- Join a patient group. You’re not alone. Thousands are managing this every day.
If you’re tired all the time, have unexplained joint pain, and your liver enzymes are high-ask your doctor about autoimmune hepatitis. Don’t let it be the last thing they check. It’s rare, but it’s treatable. And catching it early can mean the difference between a normal life and a transplant.
Is autoimmune hepatitis the same as hepatitis B or C?
No. Hepatitis B and C are caused by viruses. Autoimmune hepatitis is caused by your immune system attacking your liver. You don’t need antiviral drugs-you need immunosuppressants. The symptoms can look similar, but the treatments are completely different. Testing for viral markers is the first step in ruling out infection.
Can autoimmune hepatitis be cured?
There’s no cure yet. But many people achieve long-term remission-meaning their liver enzymes and IgG levels stay normal for years, sometimes decades, with low-dose medication. Some patients can eventually stop treatment, but only under strict medical supervision. For most, it’s a lifelong condition that requires monitoring and management.
What are the side effects of prednisone and azathioprine?
Prednisone can cause weight gain, mood swings, insomnia, high blood sugar, bone loss, and increased risk of infections. Azathioprine may lower white blood cell counts, cause nausea, or rarely lead to liver toxicity. Doctors monitor blood counts and liver enzymes regularly to catch problems early. Many patients switch to mycophenolate if side effects are too severe.
How often do I need blood tests?
During the first 3 to 6 months of treatment, you’ll need blood tests every 2 to 4 weeks to check liver enzymes and blood counts. Once you’re stable and in remission, testing usually drops to every 3 months. Skipping tests increases the risk of relapse or undetected side effects.
Can I still work and live normally with autoimmune hepatitis?
Yes, most people can-once the disease is under control. Fatigue and medication side effects can make daily life harder at first, but many patients return to work, exercise, and normal routines after 6 to 12 months of treatment. The key is consistency: taking meds, getting tests, and listening to your body. With proper management, life expectancy approaches that of someone without the disease.
Comments (15)
-
Lydia H. January 19, 2026
Man, I never realized how much this disease messes with your mental game too. I’ve been on azathioprine for three years, and yeah, the fatigue is real-but what’s worse is the guilt when you skip a blood test because you’re just too drained to care. You start feeling like a burden. Then you read something like this and remember: you’re not failing. You’re fighting.
-
Phil Hillson January 21, 2026
This post is so long I fell asleep halfway through and woke up thinking I had autoimmune hepatitis
-
Aman Kumar January 21, 2026
The clinical paradigm here is fundamentally flawed-relying on IgG titers and ANA/ASMA serology is archaic. We’re operating on 1970s immunological heuristics while ignoring the cytokine profiling and T-cell receptor clonality data that could stratify non-responders with 92% predictive accuracy. The real tragedy isn’t the disease-it’s the systemic refusal to integrate multi-omics diagnostics into routine hepatology workflows.
-
Astha Jain January 22, 2026
OMG i just found out my cousin has this and she was like ‘oh its just stress’ for 2 years 😭 like bruh its not a mood swing its your immune system eating your liver???
-
Erwin Kodiat January 22, 2026
I used to think ‘liver disease’ meant alcoholics or people who eat too much fried food. Then my sister got diagnosed at 28-never drank, vegan, runs marathons. It’s terrifying how invisible this is until it’s not. But honestly? The fact that we can control it now… that’s hope. Not a cure, but a chance. And that’s everything.
-
Christi Steinbeck January 23, 2026
If you’re reading this and you’re tired all the time-stop dismissing it. Go get your liver enzymes checked. I waited a year because I thought I was just ‘burned out.’ Turns out, I was dying slowly. Don’t be me. Get tested. You owe yourself that.
-
Valerie DeLoach January 25, 2026
One thing this post doesn’t emphasize enough: the emotional labor of being chronically ill in a world that rewards productivity. You’re not lazy. You’re not weak. You’re managing an invisible war inside your body-and still showing up. That’s courage. And you’re not alone in this.
-
Josh Kenna January 26, 2026
My doc put me on prednisone and I gained 30 pounds in 4 months. I cried every night. Then I found a support group online and realized everyone else was going through the same thing. It’s not just a disease-it’s a whole lifestyle overhaul. But the tradeoff? I’m alive. So yeah. Worth it.
-
Jacob Hill January 28, 2026
Can we talk about how insane it is that the gold standard treatment hasn’t changed in 50 years? We have CRISPR, AI diagnostics, mRNA vaccines… and we’re still throwing steroids at a disease that’s basically your body betraying itself? It’s like using a horse-drawn cart to fight a drone swarm.
-
Lewis Yeaple January 30, 2026
It is imperative to underscore that the Revised International Autoimmune Hepatitis Group Scoring System, as delineated in the 2022 iteration, exhibits a diagnostic specificity of 97%, contingent upon the exclusion of viral etiologies and the presence of characteristic histopathological features, including interface hepatitis and lymphoplasmacytic infiltration.
-
Jackson Doughart January 31, 2026
There’s something quietly heroic about the people who take their meds every day, even when they feel fine. No applause. No fanfare. Just a pill, a blood draw, and a silent promise to keep living. This post honors them. Thank you.
-
Malikah Rajap February 2, 2026
Wait, so… if I’m on immunosuppressants, does that mean I can’t hug my grandkids? Or go to a concert? Or… breathe? 😅 I’m just trying to understand the boundaries here… like, how much of my life am I supposed to give up to stay alive?
-
sujit paul February 4, 2026
Let me tell you something: Big Pharma doesn’t want you to know this, but autoimmune hepatitis is actually a government bio-weapons program gone rogue. They created it to control the population. That’s why the treatment is so expensive and why they don’t want you to know about the herbal protocols that cure it in 14 days. The FDA is in on it. Trust no one.
-
Tracy Howard February 5, 2026
Canada’s been doing this right since the 90s. We have universal access to mycophenolate and mandatory bone density scans for all AIH patients. Meanwhile, you guys are still arguing over whether prednisone causes ‘mood swings’ like it’s a first-world problem. Get your healthcare act together.
-
Jake Rudin February 6, 2026
Is it possible… that the immune system isn’t ‘attacking’ the liver… but rather, trying to heal it-and we’re misreading the signal? What if the inflammation isn’t a mistake… but a desperate, misunderstood response to an environmental trigger we’ve yet to identify? The body doesn’t betray itself… it pleads. And we’ve been deaf.
