Breathing Disorders: What They Are and How to Manage Them
If you ever felt short of breath after climbing stairs or noticed a wheeze at night, you’ve experienced a breathing disorder. These conditions affect how air moves in and out of your lungs, making everyday activities feel harder. The most common ones are asthma, chronic obstructive pulmonary disease (COPD), and allergic rhinitis that can trigger coughs. Knowing the basics helps you spot trouble early and take action before it gets serious.
Common Signs You Shouldn't Ignore
Typical symptoms include wheezing, persistent coughing, chest tightness, and a feeling of not getting enough air. Asthma often shows up with sudden attacks triggered by exercise, cold air, or allergens. COPD, usually linked to long‑term smoking, brings a chronic cough and mucus production that doesn't go away. If you notice any of these signs more than a few times a week, it’s time to track them and talk to a doctor.
Practical Steps You Can Take Today
First, identify what makes your breathing worse—dust, pollen, smoke, or even strong smells. Reducing exposure can cut down flare‑ups. Keep an inhaler handy if you have asthma; using it at the first hint of tightness often stops a full attack. For COPD, quitting smoking is the single most effective move, and staying active with gentle walks helps keep lungs flexible. Hydration matters too: drinking water thins mucus, making it easier to clear.
When you’re at home, try breathing exercises like pursed‑lip breathing or diaphragmatic breathing. They train your muscles to use air more efficiently and can calm an acute episode. Also, maintain a healthy weight; excess pounds put extra pressure on the chest and make breathing harder. If night-time symptoms disturb sleep, elevate your head with an extra pillow and keep bedroom air clean with a HEPA filter.
Medication isn’t one‑size‑fits‑all. Short‑acting bronchodilators relieve sudden tightening, while long‑term inhaled steroids reduce inflammation for asthma. COPD patients might need a combination of bronchodilators and oral meds to manage flare‑ups. Always follow the dosage your doctor prescribes—overusing rescue inhalers can actually worsen symptoms.
Lastly, keep a simple log: note when symptoms start, what you were doing, and any triggers. This record helps doctors pinpoint patterns and adjust treatment quickly. If you ever feel dizzy, faint, or can't speak full sentences because of breathlessness, treat it as an emergency and call 911.
Breathing disorders can feel overwhelming, but with the right knowledge and habits you can stay in control. Browse our related articles for deeper dives on asthma inhalers, COPD lifestyle changes, and natural ways to support lung health.
Breathing Disorders and Your Emotional Well-being: How to Stay Positive
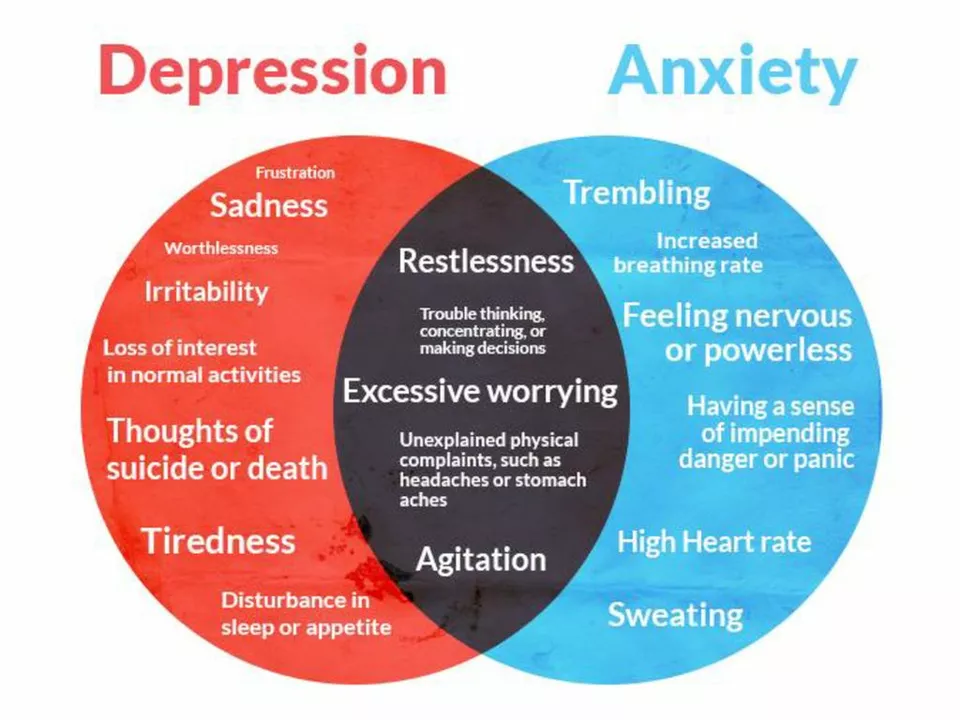
Finnegan O'Sullivan Apr 29 6Breathing disorders can significantly impact our emotional well-being, often leading to increased stress and anxiety. To stay positive, it's essential to educate ourselves on our condition, seek professional help, and develop healthy coping mechanisms. Maintaining a strong support system of friends and family is also crucial in navigating this journey. Additionally, practicing mindfulness and relaxation techniques can help improve our mental state and overall quality of life. Remember, it's vital to prioritize self-care and be patient with ourselves as we work towards better emotional well-being.
More Detail